Abstract
Two or more incidents within a six-month period or three or more within a year are considered recurrent urinary tract infections (rUTIs). With the exception of the first year of life, men to get urinary tract infections. UTIs cost the healthcare system a lot of money and cause many missed workdays. Antibiotics were once the mainstay of acute therapy; now, due to rising resistance patterns, antibiotic overuse and misuse, and a move toward antimicrobial stewardship, we are now depending increasingly on non-antibiotic and preventative measures. These are called recurrent UTIs. If they're not treated, recurrent UTIs can cause kidney damage, especially in kids younger than 6 , Berberine is the best herb for use the treatment of recurrent UTI. That are found in various plants such as European barberry and Oregon grape and the best source berberine in berberis aquifolium, that are belongs to the family of berberidaceae. Berberine is an important drug against many bacteria and combat infections by preventing the bacteria (E. coli and Proteus species) from adhering to the host cell. In this disease most common bacterial pathogen are Escherichia coli. Their treatment method are similar as the UTI. Recently cases of recurrent UTI in India 13%-14% of men will experience at least one
Keywords
Urinary tract infection, Recurrent UTI, Berberine, Aetiology, Treatment method
Introduction
UTI (Urinary tract infection): An infection that affects a portion of the urinary tract is known as a urinary tract infection (UTI) (AL, 2013). While upper urinary tract infections (pyelonephritis) damage the kidney, lower urinary tract infections (cystitis) might affect the bladder or urethra. Suprapubic pain, painful urination (dysuria), and frequent and urgent urination even when the bladder is empty are signs of a lower urinary tract infection. On the other hand, kidney infection symptoms are more systemic and typically involve flank discomfort or fever in addition to lower urinary tract infection symptoms. Rarely, blood may be seen in the urine. At the extremes of age (i.e., in individuals who are very young or old), symptoms may be ambiguous or nonspecific. (AL, 2013) (Lane DR, august 2011)
Classification: The UTI classified as two types:
1. Uncomplicated UTI
2. Complicated UTI
Uncomplicated UTI: Uncomplicated UTIs also only occur due to specific bacteria, which are behind the vast majority of cases. The urethra and bladder are also known as the lower urinary tract. Some may refer to UTIs affecting the bladder as bladder infections or cystitis. Bladder infections are the most common Trusted Source form of UTI. (Salvatore S, june2011)
Causes: Bacteria strains that could cause uncomplicated UTIs include:
- E. coli
- Klebsiella
- Proteus
- Enterobacter
- Enterococcus
E. coli and Klebsiella cause the vast majority Trusted Source of uncomplicated UTIs.
Complicated UTI: A complicated UTI is any urinary tract infection that does not fit the criteria of an uncomplicated UTI. If a doctor thinks that the UTI will be difficult to treat or could lead to complications, they will define it as a complicated UTI. (Salvatore S, june2011) A UTI can also be a complicated case if the bacteria that cause it are ones that do not typically cause UTIs.
Causes: The same bacteria that cause uncomplicated UTIs can also cause complicated UTIs. A range of different microbes can also cause complicated UTIs. This includes different bacteria and, in some cases, fungi such as Candida. Some bacteria that cause complicated UTIs may be resistant to antibiotic treatment. (Chae JH, november2015)
Sign & symptoms:
Bladder infections are another name for lower urinary tract infections. The most typical symptoms include burning when urinating, frequent urination (or the need to urinate) without vaginal discharge, and severe pain. In healthy women, these symptoms typically last six days and can range in severity from mild to severe. (Salvatore S, june2011)It's possible to have some lower back or pubic bone ache. In addition to the typical symptoms of a lower urinary tract infection, people with pyelonephritis, or upper urinary tract infection, may also have fever, nausea, and vomiting, or flank discomfort. Rarely, there may be visible pus in the urine or it may seem bloody. (Chae JH, november2015) UTIs have been associated with onset or worsening of delirium, dementia, and neuropsychiatric disorders such as depression and psychosis. However, there is insufficient evidence to determine whether UTI causes confusion (Krinitski D, (November 2021) .The reasons for this are unknown, but may involve a UTI-mediated systemic inflammatory response which affects the brain. Cytokines such as interleukin-6 produced as part of the inflammatory response may produce neuroinflammation, in turn affecting dopaminergic and/or glutamatergic neurotransmission as well as brain glucose metabolism. (Lane DR, august 2011)
Recurrent UTI (rUTI):
rUTIs are prevalent and pose a serious threat to public health and society. Both the lower and upper urinary tracts may be affected, but if upper UTIs recur frequently, a complex aetiology should be suspected. (O'Riordan, May 2023) Antibiotics have undeniable therapeutic benefits, but because of their extensive use, urinary tract infections have become more resistant. Between 20% and 50% of antibiotic prescriptions in acute hospital treatment are thought to be either unneeded or inappropriate. The goal of antimicrobial stewardship is to mitigate the consequences of these pervasive prescribing practices. (O'Riordan, May 2023) While reducing the negative impacts of antibiotic use, such as toxicity, the selection of aggressive organisms, the rise of resistant bacterial strains, and healthcare-associated infections like Clostridium difficile, it seeks to enhance therapeutic outcomes and guarantee cost-effective therapy. (a, February 2005) The WHO has declared that antimicrobial resistance (AMR) is one of the top ten global public health threats facing humanity and has developed a global action plan for AMR. (Krinitski D, (November 2021) As a result of the adherence to these principles, there is now increased interest and use of non-antibiotic adjuncts in the treatment and prophylaxis of UTIs. (O'Riordan, May 2023)
Sign and symptoms:
Symptoms of a recurrent urinary tract infection (UTI) include:
- Frequent urination, especially at night
- A sudden or urgent need to urinate
- Pain or burning while urinating
- Cloudy or bloody urine
- Pressure or cramping in the lower abdomen or back
- Difficulty emptying the bladder
- Feeling generally unwell, achy, and tired
Chronic UTIs can lead to serious complications, including kidney infections, kidney disease, sepsis, and premature delivery.
In infants and young children, signs of a UTI may be nonspecific, such as fever, vomiting, or decreased appetite or activity. Some factors that can contribute to recurrent UTIs in females include: E. coli bacteria from the rectal bacterial flora, Sexual activity, Spermicide use, and Menopause.
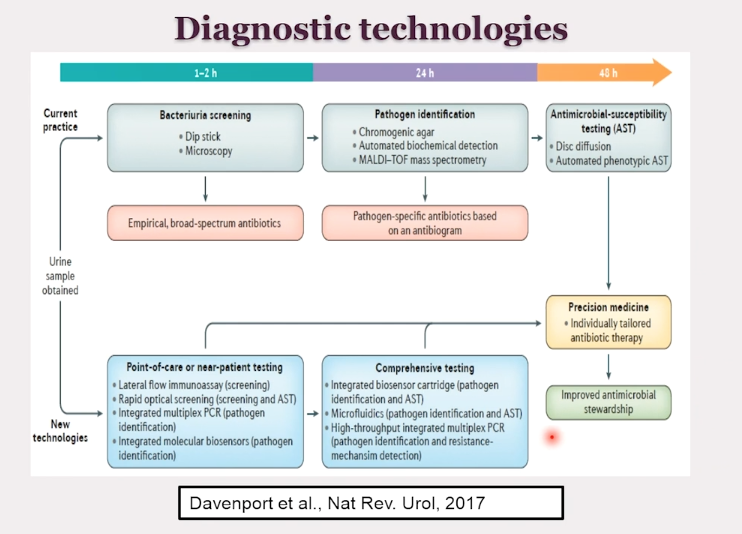
Dignosis:
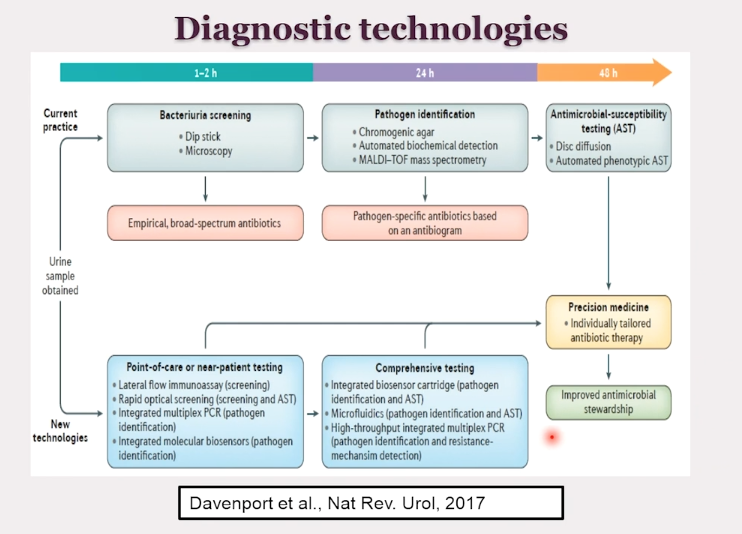
rUTIs are recurrences of uncomplicated and/or complicated UTIs (see Table 1). The spectrum of UTI ranges from self-limiting cystitis with mild symptoms to life-threatening sepsis and Fournier's gangrene (Jiang Z, September 2022). Even when mild, they can account for morbidity for the patient and account for significant time off work and regular duties. Initial diagnosis of a lower urinary tract infection is normally made clinically, with the patient presenting with features, such as new urgency, frequency, dysuria. (Amdekar S, nov2011)
Differential diagnoses:
The differential diagnosis can be determined by the patient's age and sex. Younger patients should be worked up for sexually transmitted infections (STIs) such as gonorrhoea and chlamydia. Women of child-bearing age should be considered for bacterial vaginosis and candida. Older patients are more at risk for lichen sclerosis et atrophicus and the genitourinary syndrome of menopause (formerly known as vulvo-vaginal atrophy) in postmenopausal women. (Jiang Z, September 2022)
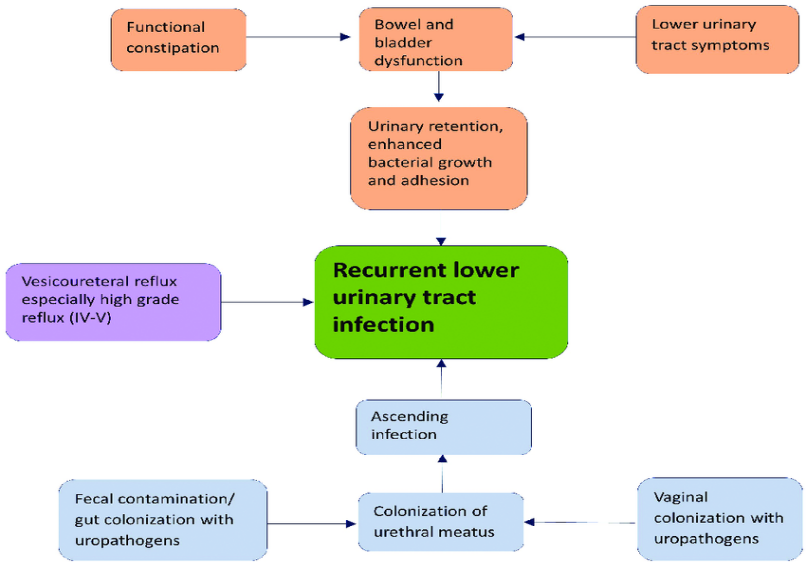
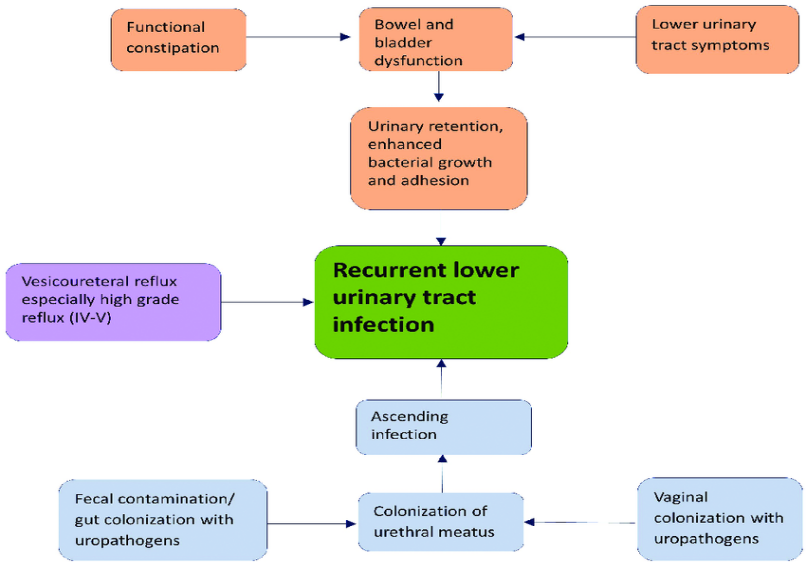
Aetiology:
Bacterial infection accounts for most UTIs, however viral and fungal infections can also occur, particularly in the immunosuppressed. The most common bacterial pathogen is Escherichia coli. Other common pathogens include Klebsiella pneumoniae, enterococcus faecalis, proteus mirabilis and pseudomonas aeruginosa (O'Riordan, May 2023). Most Gram-negative bacteria arise from the gastrointestinal tract and ascend via the urethra. It is rarer for UTI to occur as a result of haematogenous spread.
Pathogens:
The distribution of microbes in the three urine cultures necessary for the rUTI diagnosis is shown in Figure 1, the most common being Escherichia coli (41%) (O'Riordan, May 2023).
Risk Factor:
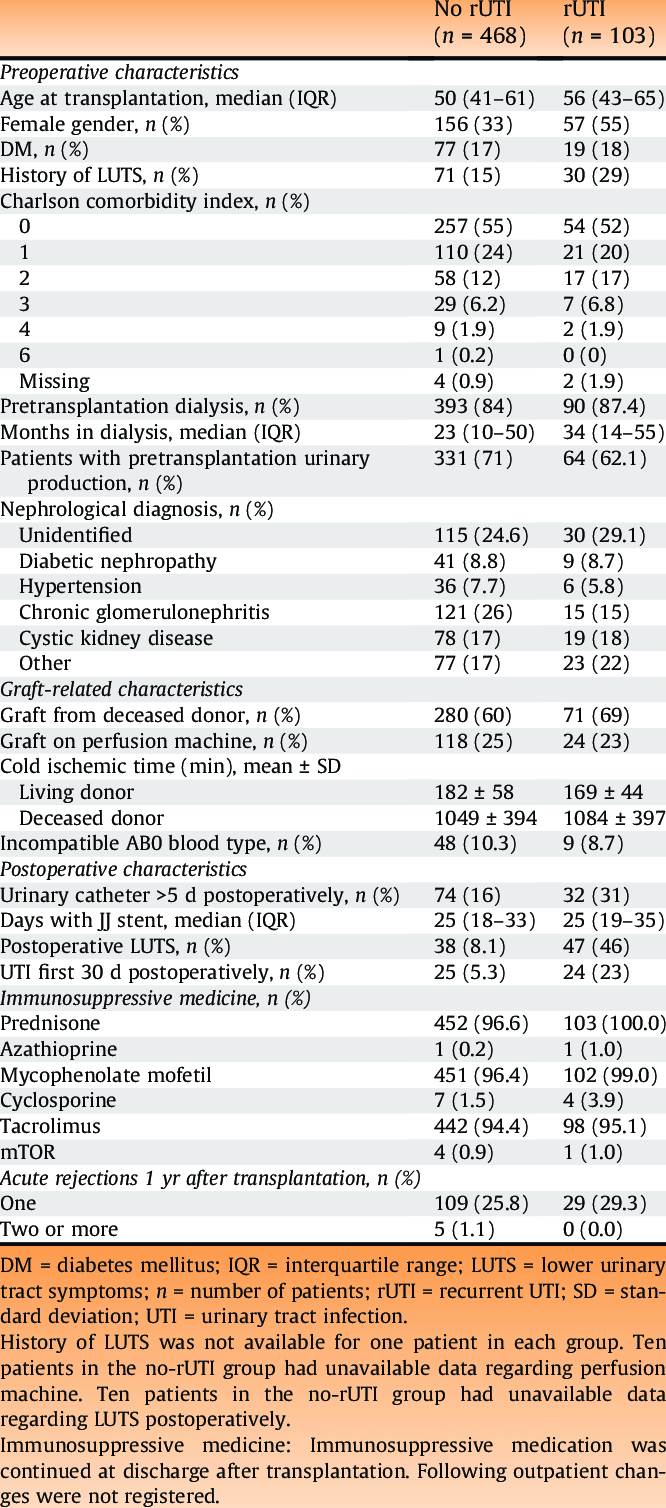
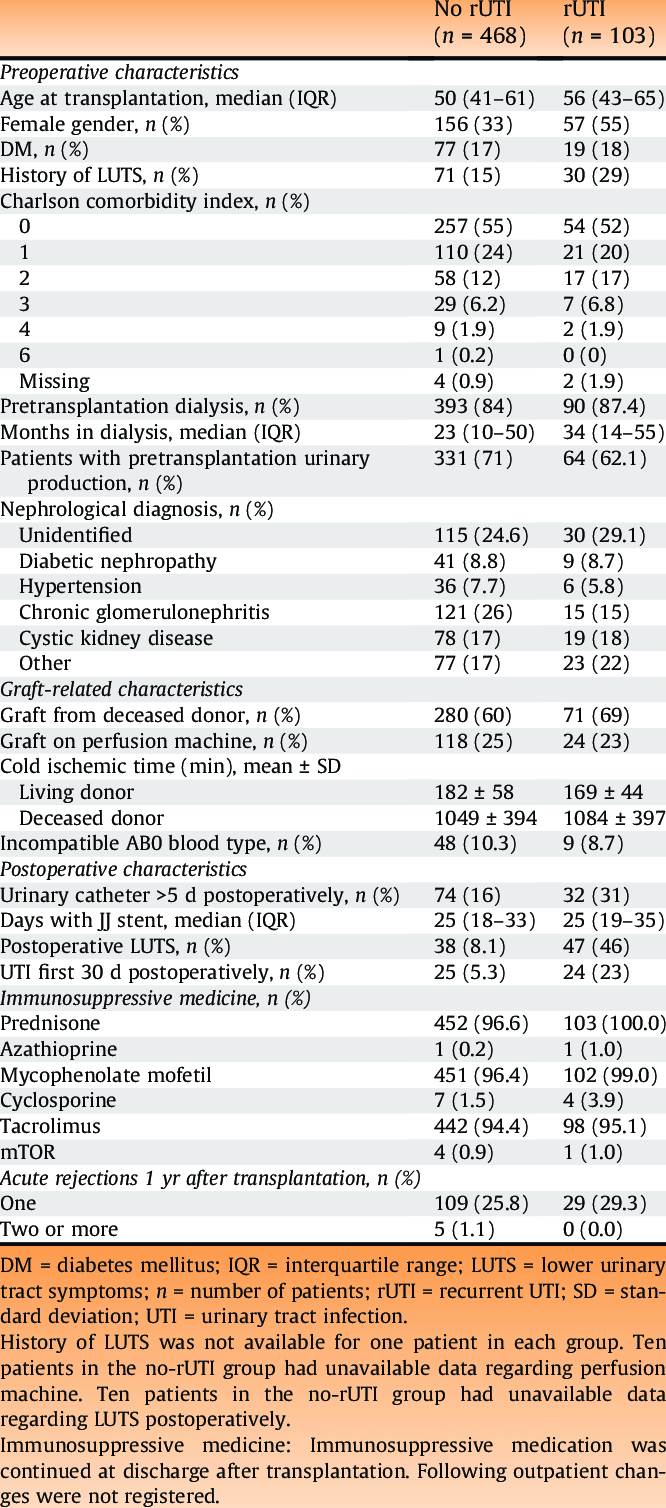
In a multivariable analysis, increasing age, female gender, and a preoperative history of lower urinary tract symptoms were significantly associated with rUTIs compared with the rest of the transplant recipients . Experiencing a UTI within the first 30 d postoperatively was the risk factor that had a strong association with an rUTI, with the highest hazard ratio. Pretransplantation urinary production, defined as <100>

Fig. 1 – Frequency of microbe groups found in the three diagnostic urine cultures for rUTI. The numbers in bars represent the absolute numbers. rUTI = recurrent urinary tract infection; UTI = urinary tract infection.
Some risk factors for recurrent urinary tract infections (UTIs) in men include:
- Immune system suppression: Conditions like diabetes or HIV can increase the risk of UTIs.
- Prostate problems: An enlarged prostate can block urine flow, leading to a buildup of bacteria and UTIs.
- Kidney stones: Kidney stones can cause urine to build up in the bladder, increasing the risk of UTIs.
- Catheter use: Catheters increase the risk of UTIs because they allow urine to be emptied when a person can't urinate on their own.
- Recent procedures: Urinary tract surgery or exams using medical instruments can increase the risk of UTIs.
- Sexually transmitted diseases (STDs): STDs like chlamydia and gonorrhea can cause UTIs.
- Unprotected sex: Having multiple sex partners or having sex without a condom increases the risk of STIs and UTIs.
- Poor hygiene: Poor hygiene can increase the risk of UTIs.
- Urinary tract abnormalities: Some anatomical defects can prevent urine from leaving the body normally or cause urine to back up in the urethra.
Table 1 – Clinical characteristics of the cohort, stratified for patients with or without rUTIs
Treatment strategies for managing recurrent UTIs:
Strategies include behavioural modifications, such as avoidance of risk factors; non-antibiotic options and antibiotic options.
Behavioural modifications are commonly recommended but these practices are not strongly supported by evidence. It is known that sexually active women and those who use spermicides are more likely to be at risk of a UTI. Behavioural modifications can play a role here. Other recommendations, although likely apocryphal, include optimizing diabetic control, timed voiding, avoidance of diaphragm use, post-coital voiding, wiping from front to back after defaecation and the wearing of cotton. (O'Riordan, May 2023)
Post-menopausal women tend to develop changes to their oestrogen-sensitive tissues such as the vulva, vagina and urethra. This can lead to a reduction in host factors which protect against UTI. The epithelium thins, tends to crack, loses elasticity and becomes dry, the pH rises, the numbers of normal commensal lactobacilli diminish, leading to an overgrowth in pathogenic bacteria. This is called the genitourinary syndrome of menopause (GSM) (formerly vulvovaginal atrophy) (O'Riordan, May 2023).
Treatment and further examination:
In the rUTI patient group, 39 (38%) were started on prophylactic antibiotic treatment after the rUTI diagnosis to prevent further UTIs. The most used were pivmecillinam (64%), trimethoprim (15%), nitrofurantoin (7.7%), and ciprofloxacin (7.7%). Local estrogen was given to 22 (39%) of female recipients as a prophylactic measure for rUTIs. (b, June 2023) A total of 57 of 103 patients were referred for a urological workup for further examination of their underlying pathophysiology. Male patients (33 of 46) with rUTIs were referred to a urologist more often than females (24 of 57). Fifteen of 57 female recipients with rUTIs were referred to a gynecologist. (O'Riordan, May 2023) Thirty of the total 57 female recipients with rUTIs were referred to a urologist and/or gynecologist, and some were referred to both.
The urological examinations included cystoscopy (79%), flow and residual urine test (71%), computed tomographic urography (32%), and urodynamic test (21%). Urological workup resulted in a diagnosis of 26 patients, of whom 16 (28%) were diagnosed with residual urine although no strict definition was used, five (8.8%) with benign prostatic hyperplasia, two (3.5%) with urethral stricture, two (3.5%). (b, June 2023)
- Treatment for an acute, symptomatic UTI
Antibiotic choice is guided by:
- Spectrum and susceptibility patterns of the pathogens.
- Efficacy for the particular indication in clinical studies.
- Tolerability and adverse reactions.
- Adverse ecological effects.
- Costs,Availability.
There are many patent factors which need to be taken into consideration when prescribing antibiotics. These include drug allergies, renal/hepatic function, presence of interacting drugs, comorbidities, age, pregnancy and host-immune function (b, June 2023).
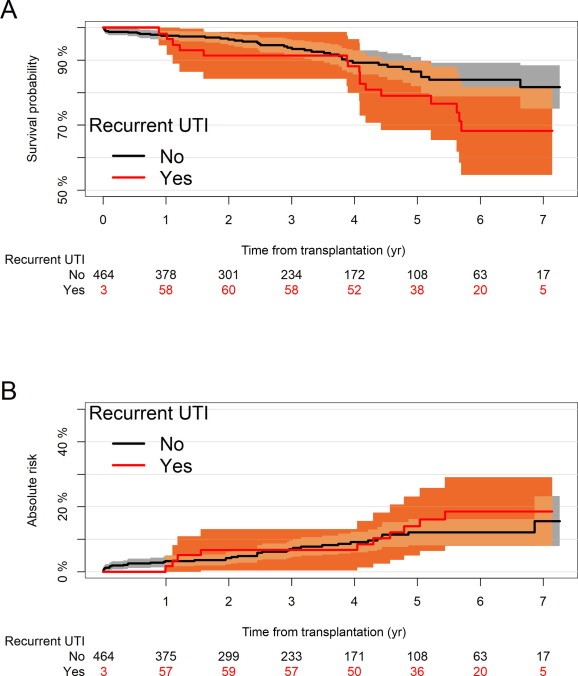
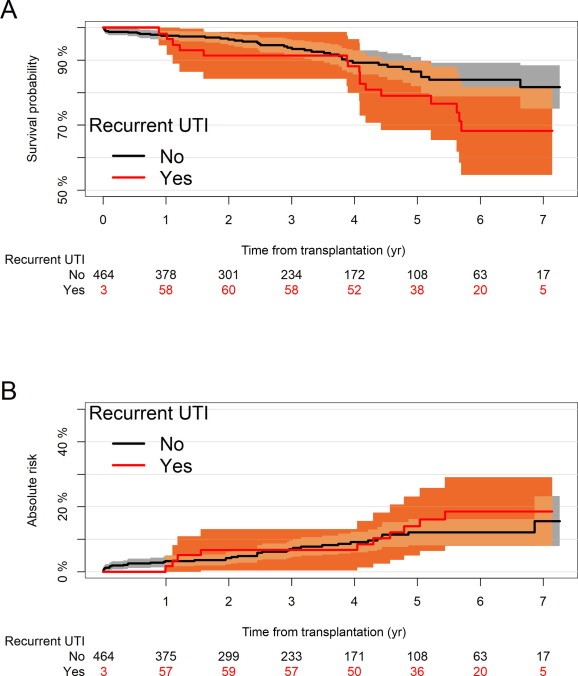
Fig. 2 – (A) Cumulative incidence of graft loss, with death as a competing risk. (B) Kaplan-Meier plot on overall patient survival comparing patients having rUTI with those having no rUTI. The analysis is adjusted for the immortality bias by delayed entry in the recurrent UTI group. Be aware that the Y axis shows a limit of 50%. rUTI = recurrent urinary tract infection; UTI = urinary tract infection.
Treatment method for recurrent UTI (rUTI):
Treatment method for recurrent urinary tract infections (UTIs) can include:
- Antibiotics
- Vaginal estrogen cream
- Non-antibiotic therapies
- Vaccines
Some other tips to prevent UTIs include: Wiping from front to back, Urinating before and after sex, Drinking lots of water, and Avoiding tight underpants and jeans (AL, 2013).
Drugs used in treatment of recurrent UTI:
Antibiotics are commonly used to treat urinary tract infections (UTIs) in men, and the preferred drugs for recurrent UTIs include:
- Nitrofurantoin: 50–100 mg taken before bed daily
- Sulfamethoxazole-trimethoprim: 40/200 mg taken before bed daily
- Trimethoprim: 100 mg taken before bed daily
Other antibiotics used to treat UTIs include:
- Fosfomycin (Monurol)
- Cephalexin
- Ceftriaxone
- Amoxicillin
- Doxycycline
- Quinolones, such as ciprofloxacin or levofloxacin
Adult men with UTIs should take antibiotics for 10–14 days. Phenazopyridine can be used to treat the symptom of dysuria (Chae JH, november2015).
Carbapenems are another type of antibiotic that are often considered a drug of last resort. Common side effects include nausea and vomiting. At high doses, these drugs can cause seizures, especially imipenem (AL, 2013).
Herbal Medicines (Phytoconstituent):
Berberine is an important drug against many bacteria and combat infections by preventing the bacteria (E. coli and Proteus species) from adhering to the host cell, which suggests their potent role in treating rUTI. Berberine, a compound found in various plants, such as European barberry and Oregon grape, has a long history of medicinal use dating back over 3,000 years. It has potential benefits in treating conditions such as recurrent UTI, diabetes, high cholesterol etc.
- The best source of Berberine in Berberis aquifolium (Oregon grape)
Berberine dosage
The suggested dose of berberine is 250 milligrams or 500 milligrams two or three times a day.
Management of recurrent UTI (rUTI):
Recurrent urinary tract infections (rUTIs) can be managed with a combination of behavioral changes, antibiotics, and other treatments:
For women with cystitis associated with sexual activity, postcoital antibiotics can be taken to reduce the risk of adverse effects. For other cases, continuous prophylaxis may be recommended. Some common antibiotics used for prophylaxis include Bactrim, Fosfomycin, and Nitrofurantoin.
Some studies have shown that cranberry juice or tablets can reduce the number of symptomatic UTIs over a 12-month period. However, other studies have found that cranberry juice is not effective in preventing rUTIs.
This can be recommended for postmenopausal women with vulvovaginal atrophy.
Patients with a PVR volume greater than 50–100 mL may benefit from conservative measures to reduce PVR, such as pelvic floor exercises or relaxation techniques.
These include drinking at least 2 liters of fluids per day, wiping from front to back, and avoiding reusable sponges and luffas.
Some patients may need to be referred to a urologist for further investigation or other treatment strategies.
Surgical management:
Urethral dilatation is a traditional treatment for prevention of rUTI although it lacks robust evidence. Future therapies may involve the use of intravaginal laser in an attempt to replenish normal vaginal defences by boosting collagen production. Some patients may need to be referred to a urologist for further investigation or other treatment strategies.
Cases of recurrent UTI in MEN in India:
Although recurrent UTIs are more common in women, around 20% of all diagnosed UTI cases occur in men. Despite the lower incidence, approximately 13–14% of men will experience at least one UTI in their lifetime, compared to around 50% of women (Sarita Mohapatra 1, 2022 Feb ).
CONCLUSION:
Preventing rUTIs is probably an unattainable goal. Instead, our focus should be on reducing the number of recurrent UTIs and morbidity associated with them. Our armamentarium has expanded exponentially and the single-pronged approach of treatment dose-antibiotics is now something of the past. Patients and clinicians now have several strategies to reduce the recurrence of UTIs ranging from behavioural modifications, non-antibiotic treatments and different regimens of antibiotic treatments. One in six patients experience rUTIs after RTx. Pre- and postoperative variables affect the risk of rUTIs, but none are easily modifiable. In this cohort, rUTIs did not affect the graft function or survival. The etiology of rUTIs remains poorly understood, and there is a continuous need to study how rUTIs can be reduced and treated optimally. There are several risk factors that can guide early detection and management. We could not demonstrate an effect of rUTIs on graft or patient survival. Also in this cohort, but is not necessarily different from the background population. Besides the above statistical result-based conclusions, this complex UTI clinic service also reinforced that clinical history is crucial and exploring the drug allergies to assess their severity is vital to not miss out on potential treatment options through a risk versus benefit analysis. MDT approach (involving the microbiologists) adds a different perspective and dimension to management
REFERENCE
- "Urinary Tract Infection". Centers for Disease Control and Prevention (CDC). 17 April 2015. Archived from the original on 22 February 2016. Retrieved 9 February 2016.
- Jump up to:a b c d e Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ (May 2015). "Urinary tract infections: epidemiology, mechanisms of infection and treatment options". Nature Reviews. Microbiology. 13 (5): 269–284. doi:10.1038/nrmicro3432. PMC 4457377. PMID 25853778.
- Jump up to:a b c d e f g Colgan R, Williams M, Johnson JR (September 2011). "Diagnosis and treatment of acute pyelonephritis in women". American Family Physician. 84 (5): 519–526. PMID 21888302.
- Jump up to:a b c d e f g h i j k l m n o p q r s t u v w x Nicolle LE (February 2008). "Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis". The Urologic Clinics of North America. 35 (1): 1–12, v. doi: 10.1016/j.ucl.2007.09.004. PMID 18061019.
- Salvatore S, Salvatore S, Cattoni E, Siesto G, Serati M, Sorice P, Torella M (June 2011). "Urinary tract infections in women". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 156 (2): 131–136. doi: 10.1016/j.ejogrb.2011.01.028. PMID 21349630
- Lane DR, Takhar SS (August 2011). "Diagnosis and management of urinary tract infection and pyelonephritis". Emergency Medicine Clinics of North America. 29 (3): 539–552. doi: 10.1016/j.emc.2011.04.001. PMID 21782073.
- Jump up to:a b c d e Woodford HJ, George J (February 2011). "Diagnosis and management of urinary infections in older people". Clinical Medicine. 11 (1): 80–83. doi:10.7861/clinmedicine.11-1-80. PMC 5873814. PMID 21404794.
- Study Guide for Pathophysiology (5 ed.). Elsevier Health Sciences. 2013. p. 272. ISBN 9780323293181. Archived from the original on 16 February 2016.
- Introduction to Medical-Surgical Nursing. Elsevier Health Sciences. 2015. p. 909. ISBN 9781455776412. Archived from the original on 11 January 2023. Retrieved 17 September 2017.
- Jarvis WR (2007). Bennett & Brachman's hospital infections (5th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 474. ISBN 9780781763837. Archived from the original on 16 February 2016.
- Ferroni M, Taylor AK (November 2015). "Asymptomatic Bacteriuria in Noncatheterized Adults". The Urologic Clinics of North America. 42 (4): 537–545. doi: 10.1016/j.ucl.2015.07.003. PMID 26475950.
- Glaser AP, Schaeffer AJ (November 2015). "Urinary Tract Infection and Bacteriuria in Pregnancy". The Urologic Clinics of North America. 42 (4): 547–560. doi: 10.1016/j.ucl.2015.05.004. PMID 26475951.
- Jump up to:a b c "Recurrent uncomplicated cystitis in women: allowing patients to self-initiate antibiotic therapy". Prescrire International. 23 (146): 47–49. February 2014. PMID 24669389.
- Lee JH, Kim SW, Yoon BI, Ha US, Sohn DW, Cho YH (January 2013). "Factors that affect nosocomial catheter-associated urinary tract infection in intensive care units: 2-year experience at a single center". Korean Journal of Urology. 54 (1): 59–65. doi:10.4111/kju.2013.54.1.59. PMC 3556556. PMID 23362450.
- Jump up to:a b c d e f Colgan R, Williams M (October 2011). "Diagnosis and treatment of acute uncomplicated cystitis". American Family Physician. 84 (7): 771–776. PMID 22010614.
- Jump up to:a b c Al-Achi A (2008). An introduction to botanical medicines: history, science, uses, and dangers. Westport, Conn.: Praeger Publishers. p. 126. ISBN 978-0-313-35009-2. Archived from the original on 28 May 2016.
- Arellano RS (19 January 2011). Non-vascular interventional radiology of the abdomen. New York: Springer. p. 67. ISBN 978-1-4419-7731-1. Archived from the original on 10 June 2016.
- Jump up to:a b c Chae JH, Miller BJ (November 2015). "Beyond Urinary Tract Infections (UTIs) and Delirium: A Systematic Review of UTIs and Neuropsychiatric Disorders". Journal of Psychiatric Practice. 21 (6): 402–411. doi:10.1097/PRA.0000000000000105. PMID 26554322. S2CID 24455646.
- Jump up to:a b c Krinitski D, Kasina R, Klöppel S, Lenouvel E (November 2021). "Associations of delirium with urinary tract infections and asymptomatic bacteriuria in adults aged 65 and older: A systematic review and meta-analysis". Journal of the American Geriatrics Society. 69 (11): 3312–3323. doi:10.1111/jgs.17418. PMC 9292354. PMID 34448496.
- Balogun SA, Philbrick JT (March 2014). "Delirium, a Symptom of UTI in the Elderly: Fact or Fable? A Systematic Review". Canadian Geriatrics Journal. 17 (1): 22–26. doi:10.5770/cgj.17.90. PMC 3940475. PMID 24596591.
- Mayne S, Bowden A, Sundvall PD, Gunnarsson R (February 2019). "The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing - a systematic literature review". BMC Geriatrics. 19 (1): 32. doi:10.1186/s12877-019-1049-7. PMC 6360770. PMID 30717706.
- Jump up to:a b Rashid MH, Sparrow NA, Anwar F, Guidry G, Covarrubias AE, Pang H, et al. (October 2021). "Interleukin-6 mediates delirium-like phenotypes in a murine model of urinary tract infection". Journal of Neuroinflammation. 18 (1): 247. doi:10.1186/s12974-021-02304-x. PMC 8554965. PMID 34711238.
- Jump up to:a b Jiang Z, Liang F, Zhang Y, Dong Y, Song A, Zhu X, et al. (September 2022). "Urinary Catheterization Induces Delirium-Like Behavior Through Glucose Metabolism Impairment in Mice". Anesthesia and Analgesia. 135 (3): 641–652. doi:10.1213/ANE.0000000000006008. PMC 9388475. PMID 35389369
- Jean O'Riordan, Jeremy Ockrim et al. Management of recurrent urinary tract infections in adults Volume 41, Issue 5, May 2023, https://doi.org/10.1016/j.mpsur.2023.02.011
- Anna C.L. Halskov et al. Incidence of and Risk Factors for Recurrent Urinary Tract Infections in Renal Transplant Recipients Volume 52, June 2023 https://doi.org/10.1016/j.euros.2023.04.001
- M.E. Hulscher et al. Antibiotic prescribing in hospitals: a social and behavioural scientific approach Lancet Infect Dis 2010)
- E.P. van Haarst et al. Evaluation of the diagnostic workup in young women referred for recurrent lower urinary tract infections Urology (2001)
- Y.Y. Chen et al. Estrogen for the prevention of recurrent urinary tract infections in postmenopausal women: a meta-analysis of randomised controlled trials Int Urogynecol J (2021)
- G.M. Pinggera et al. Effects of local estrogen therapy on recurrent urinary tract infections in young females under oral contraceptives Eur Urol (2005)
- A.J. Schaeffer et al. Efficacy and safety of self-start therapy in women with recurrent urinary tract infections J Urol (1999)
- Aydin A, Ahmed K, Zaman I, Khan MS, Dasgupta P. Recurrent urinary tract infections in women. Int Urogynecol J. 2015 Jun;26(6):795-804. [PubMed]
- Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002 Jul 08;113 Suppl 1A:5S-13S. [PubMed]
- Anger J, Lee U, Ackerman AL, Chou R, Chughtai B, Clemens JQ, Hickling D, Kapoor A, Kenton KS, Kaufman MR, Rondanina MA, Stapleton A, Stothers L, Chai TC. Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. J Urol. 2019 Aug;202(2):282-289. [PubMed]
- Nishant Aggarwal; Stephen W. Leslie; Saran Lotfollahzadeh. Recurrent Urinary Tract Infections May 2, 2024.
- P Chitteti 1, I Ekpeno 1, J Morris,Laverick 1, S Bezemer 1, V McCune 1, I Kubelka 1, M Nadeem. 82 - Treatment outcomes among patients with recurrent Urinary Tract Infections using a multidisciplinary management approach in a complex UTI clinic- A 2-year experience Volume 12, Supplement, October 2024 https://doi.org/10.1016/j.cont.2024.101424
- Suthanthiran M, Strom TB. Renal transplantation. N Engl J Med 2010; 331:365–76.
- Chaudhry D, Chaudhry A, Peracha J, Sharif A. Survival for waitlisted kidney failure patients receiving transplantation versus remaining on waiting list: systematic review and meta-analysis. BMJ 2022;376: e068769.
- Streeter EH, Little DM, Cranston DW, Ris PJM. The urological complications of renal transplantation: a series of 1535 patients. BJU Int 2002; 90:627–34.
- Dinckan A, Tekin A, Turkyilmaz S, et al. Early and late urological complications corrected surgically following renal transplantation. Transplant Int 2007; 20:702–7


 HARI PRASAD SONWANI*
HARI PRASAD SONWANI*
 GUMAN
GUMAN
 SHWETA KUMARI SAW
SHWETA KUMARI SAW
 JAYVANT SAHU
JAYVANT SAHU
 Upasana Sahu
Upasana Sahu

 10.5281/zenodo.14846234
10.5281/zenodo.14846234