Abstract
Schizophrenia is a complex neurological disorder characterized by a distorted perception of reality, disorganized thought processes, and impaired social interaction. It is a chronic condition that can significantly impact an individual’s quality of life. The exact etiology of schizophrenia remains unclear, but it is believed to involve a combination of genetic, environmental, and neurobiological factors. Schizophrenia is a complex neurological disorder characterized by a range of cognitive, emotional, and behavioral symptoms. The condition is typically diagnosed in late adolescence or early adulthood and can significantly impair an individual’s ability to function in daily life.
Keywords
Dopamine, Neurological, Schizophrenia, Sustained, Therapeutic.
Introduction
Schizophrenia, a debilitating mental illness, was initially described by Kraepelin in 1896 as “dementia praecox” and later renamed by Bleuler in 1911. Characterized by disturbances in thought, perception, and affect, this condition significantly impacts an individual’s sense of self and agency. In 1959, Schneider identified first-rank symptoms, including auditory hallucinations, passivity experiences, and delusional thinking, which are core manifestations of schizophrenia.
Schizophrenia is a mental health problem that makes it hard to tell the difference between what is real and what is not real. People with schizophrenia may also have disorganized thoughts and problems with social interactions. Long-acting medications (LAMs) have emerged as a significant treatment option for individuals with schizophrenia, offering several advantages over oral medications. LAMs are administered through injection, typically every 2-3 weeks, providing a sustained release of medication into the bloodstream. This sustained release helps maintain therapeutic levels of medication, reducing the risk of relapse and improving treatment adherence. Unlike oral medications, which may be forgotten or intentionally missed, LAMs ensure consistent medication delivery, leading to better outcomes for patients. One of the primary benefits of LAMs is their ability to reduce the symptoms of schizophrenia. By maintaining consistent medication levels, LAMs can help manage hallucinations, delusions, disorganized thoughts, and other psychotic symptoms. This can lead to improved quality of life for individuals with schizophrenia, allowing them to participate more fully in social and occupational activities. In addition to symptom management, LAMs can also play a role in preventing relapse. Studies have shown that individuals who consistently take LAMs have a lower risk of experiencing a relapse of their psychotic symptoms. This is particularly important for individuals with schizophrenia, as relapses can be associated with significant functional impairment and increased hospitalization rates.
While LAMs offer several advantages, it is important to note that they are not suitable for everyone with schizophrenia. Some individuals may prefer oral medications or may have contraindications that make LAMs inappropriate. It is essential to discuss the potential benefits and risks of LAMs with a healthcare professional to determine the most appropriate treatment plan. Furthermore, it is important to emphasize that LAMs are not a cure for schizophrenia. They are a valuable tool for managing the symptoms of the condition and reducing the risk of relapse. However, they often need to be combined with other forms of treatment, such as psychotherapy, to address the broader social and emotional challenges faced by individuals with schizophrenia.
Etiology of Schizophrenia:
Despite extensive research spanning over a century, the definitive cause of schizophrenia remains elusive to investigators. However, there is a consensus that the diverse manifestations of the disorder stem from a complex interplay of genetic predisposition and environmental factors.
One hypothesis suggests that the onset of schizophrenia may originate during the prenatal period. Obstetrical complications, such as bleeding during pregnancy, gestational diabetes, emergency cesarean section, asphyxia, and low birth weight, have been implicated as potential risk factors for the development of schizophrenia later in life. Fetal disturbances occurring during the second trimester, a critical phase of neurodevelopment, have garnered particular attention from researchers. Infections and elevated stress levels experienced by the mother during this period have been associated with a twofold increase in the likelihood of offspring developing schizophrenia.
Scientific research provides compelling evidence that genetic factors significantly contribute to the development of schizophrenia. Numerous studies have consistently demonstrated a heightened risk of the illness among individuals with a family history. First-degree relatives, such as parents and siblings, have approximately a 10% chance of developing schizophrenia, while the risk for second-degree relatives, including grandparents and aunts, is approximately 3%. Monozygotic twins, who share identical genetic material, exhibit a significantly higher concordance rate for schizophrenia, with a 48% likelihood of both twins being affected. In contrast, dizygotic twins, who share only half of their genetic material, have a lower concordance rate of 12% to 14%. Additionally, when both parents have schizophrenia, the risk of their offspring developing the disorder is approximately 40%.
To investigate the relative influence of genetic and environmental factors, studies of adopted children have been conducted. These investigations have consistently indicated that the risk of schizophrenia is primarily determined by genetic inheritance from biological parents, rather than environmental factors experienced during childhood. This genetic basis is further supported by the observation that siblings with schizophrenia often experience similar ages of onset, suggesting a shared genetic predisposition.
Environmental and socioeconomic factors may contribute to the development of schizophrenia, particularly in individuals with genetic vulnerability. Childhood trauma, minority ethnicity, urban residence, and social isolation are among the environmental stressors associated with schizophrenia. Moreover, social stressors, such as discrimination or economic hardship, may increase the likelihood of delusional or paranoid ideation.
Epidemiology of Schizophrenia:-
Opit (1994) elucidates the methodological challenges inherent in epidemiological studies, cautioning against premature causal inference. The reliance on inductive reasoning in epidemiology often leads to an oversight of the “limits of inference,” which are significantly influenced by the specific methodology employed. Jabelensky (1993) echoes these concerns, particularly in the context of Schizophrenia. The hypothetical nature of the disease concept and the absence of validated objective markers pose substantial methodological hurdles in schizophrenia research. The ensuing review is presented with these considerations in mind. The World Health Organization’s ten-country study on the prevalence and course of schizophrenia (Jabelensky et al., 1992) revealed a consistent incidence rate of 0.7 to 1.4 per 10,000 population across diverse cultural contexts. The latter, in particular, has significantly influenced the classification and diagnosis of schizophrenia over the past two decades. As highlighted by Taylor and Abrams (1978), the stability of prevalence rates suggests that changes in diagnostic practices have played a more prominent role than actual shifts in the incidence of the disorder.
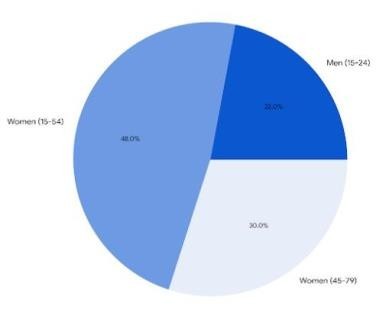
The World Health Organization's Investigation (Jabelensky et al., 1993) identified a preponderance of males in the age bracket of 15 to 24 years when examining initial contacts for schizophrenia, whereas females were disproportionately represented in the age range of 15 to 54 years. This study concluded that the lifetime risk (15-54 years) for the illness was comparable between both sexes. Haffner et al. (1993) delved into the impact of age and sex on the onset of schizophrenia in a German cohort of 267 individuals with schizophrenia. The mean age at onset exhibited a disparity of three to four years in this sample, with the age distribution revealing a sharp increase up to 25 years in males and a subsequent peak in females between the ages of 45 and 79 years.
The prevalence of schizophrenia within the United States population ranges from 0.6% to 1.9%. Furthermore, a long-acting injectable MS analysis has indicated that the annual diagnosed prevalence of schizophrenia in the United States is 5.1 per 1,000 individuals. Although the incidence of the disorder appears to be equivalent in males and females, the onset of symptoms tends to occur at an earlier age in males. Males frequently experience their initial episode of schizophrenia in their early twenties, whereas females typically encounter their first episode in their late twenties or early thirties. Research investigating a potential correlation between the geographic location of birth and the development of schizophrenia has yielded inconclusive findings. A collaborative study conducted by the World Health Organization across ten countries revealed that schizophrenia occurred with Comparable frequencies among the various geographically defined populations. Conversely, a more recent review, encompassing data from thirty-three countries, concluded that the incidence of schizophrenia exhibited geographical variation.

Fig 2: Epidemiology based on gender
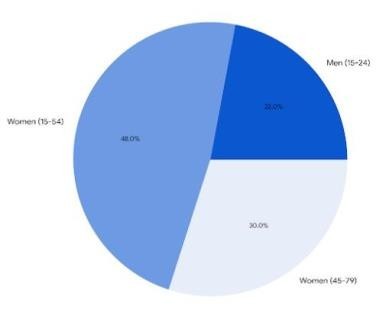
Fig 3: Age Distribution of Schizophrenia onset
Pathophysiology of Schizophrenia:
The pathophysiology of schizophrenia has been extensively explored, with theories often centering on neurotransmitter imbalances. While dopamine, serotonin, and glutamate have been extensively studied, other neurotransmitters such as aspartate, glycine, and GABA have also been implicated. Among these, abnormal activity at dopamine receptor sites, particularly D2, is believed to be associated with many of the symptoms of schizophrenia. Four distinct dopaminergic pathways have been identified: the nigrostriatal, mesolimbic, mesocortical, and tuberoinfundibular pathways. Alterations in dopamine levels within these pathways are hypothesized to contribute to the various symptoms of schizophrenia, including motor disturbances, positive symptoms, negative symptoms, cognitive deficits, and hormonal changes.
The serotonin hypothesis of schizophrenia emerged following the discovery that lysergic acid diethylamide (LSD) amplified serotonin’s effects within the brain. Subsequent research led to the development of drug compounds that antagonized both dopamine and serotonin receptors, representing a departure from older medications that exclusively targeted dopamine receptors. These newer compounds demonstrated efficacy in mitigating both the positive and negative symptoms of schizophrenia.

Fig 4: Pathophysiology of Schizophrenia
An alternative theory posits a role for glutamate, the primary excitatory neurotransmitter in the brain, in the etiology of schizophrenia. This theory gained traction from the observation that phenylcyclidine and ketamine, noncompetitive NMDA/glutamate antagonists, induce schizophrenia-like symptoms. This finding suggested a potential dysfunction in NMDA receptors in the regulation of mesocortical dopamine neurons, offering a plausible explanation for the negative, affective, and cognitive symptoms experienced by individuals with schizophrenia.
Neuroanatomical alterations have also been identified in individuals with schizophrenia. Beyond an enlargement of the third and lateral ventricles, those at high risk of a schizophrenic episode exhibit a reduced medial temporal lobe volume.
Risk Factors of Schizophrenia:
1. Genetic factors:
Schizophrenia is a complex mental health condition with a significant genetic component. While environmental factors also play a role, genetic predisposition is a major contributor. Here’s a breakdown of the genetic factors involved:
I] Familial Risk -
a) Heritability: Studies have consistently shown that schizophrenia has a strong genetic component. The risk of developing schizophrenia is significantly higher in individuals with a family history of the disorder.
b) First-degree relatives: Individuals with a parent or sibling diagnosed with schizophrenia have a significantly increased risk compared to the general population.
II] Twin Studies -
a) Monozygotic twins: Identical twins share 100% of their genetic material. If one twin develops schizophrenia, the other has a significantly higher risk compared to fraternal twins (who share only 50% of their genetic material).
b) Dizygotic twins: Fraternal twins have a lower concordance rate for schizophrenia than identical twins, further supporting the genetic influence.
III] Genome-Wide Association Studies (GWAS)
a) Multiple genes: GWAS has identified numerous genetic variants associated with schizophrenia. These studies have revealed that the disorder is likely influenced by a complex interplay of multiple genes rather than a single gene.
b) Polygenic risk scores: By combining information from multiple genetic variants, researchers can calculate polygenic risk scores, which provide estimates of an individual’s risk for developing schizophrenia based on their genetic makeup.
IV] Copy Number Variants (CNVs) -
a) Deletions or Duplications: CNVs are variations in the number of copies of a particular DNA sequence. They can involve deletions or duplications of large segments of DNA.
b) Disruption of Gene Function: CNVs can disrupt the function of genes involved in brain development and neurotransmission.
c) Structural variations: CNVs are large-scale deletions or duplications of DNA segments. Certain CNVs have been linked to an increased risk of schizophrenia, suggesting that structural variations in the genome can contribute to the disorder.
V] Epigenetics -
a) Gene expression: Epigenetics refers to changes in gene expression that do not involve alterations to the DNA sequence. Environmental factors can influence
epigenetic modifications, which can affect the development and function of the brain.
b) Gene-environment interactions: Epigenetic mechanisms may mediate the interaction between genetic susceptibility and environmental factors in the development of schizophrenia.
2. Environmental factors:
I] Childhood Trauma:
a) Abuse: Physical, emotional, or sexual abuse during childhood can increase the vulnerability to schizophrenia.
b) Neglect: Neglectful parenting can also contribute to the development of the disorder.
II] Urban Environment:
a) Pollution: Exposure to air pollution, particularly in urban areas, has been linked to an increased risk of schizophrenia.
b) Stressful Living Conditions: Crowded living conditions and social isolation can contribute to the development of schizophrenia.
III] Substance Abuse
a) Cannabis: Early-onset cannabis use has been shown to increase the risk of developing schizophrenia in individuals with a genetic predisposition.
b) Other Substances: Excessive use of other substances, such as alcohol and illicit drugs, can exacerbate symptoms of schizophrenia.
IV] Stress -
a) Life Events: Major life stressors, such as job loss, relationship breakups, or financial difficulties, can trigger or worsen symptoms of schizophrenia.
b) Chronic Stress: Long-term stress can also contribute to the development and progression of the disorder.
V] Migration -
a) Cultural Factors: Migration to a new culture can be stressful and increase the risk of developing schizophrenia, particularly if there is a lack of social support.
b) Discrimination: Experiences of discrimination or prejudice can also contribute to the onset of schizophrenia.
3. Neurobiological Factors Affecting Schizophrenia:
I] Genetic Predisposition
a) Heritability: Schizophrenia has a significant genetic component, with family studies demonstrating a higher prevalence among relatives of individuals with the disorder.
b) Polygenic Inheritance: Multiple genes are likely involved, each contributing a small effect to the overall risk.
c) Gene-Environment Interactions: Genetic factors may interact with environmental influences, such as stress or exposure to toxins, to increase susceptibility.
2] Neurotransmitter Dysregulation -
a) Dopamine Hypothesis: The dopamine hypothesis posits that excessive dopamine activity in certain brain regions, particularly the mesolimbic system, is associated with the positive symptoms of schizophrenia, such as hallucinations and delusions.
b) Glutamate Dysfunction: Evidence suggests that alterations in glutamate signaling, a key excitatory neurotransmitter, may contribute to cognitive deficits and negative symptoms in schizophrenia.
c) Serotonin Imbalance: Serotonin, a neurotransmitter involved in mood regulation, has also been implicated in the disorder, particularly in negative symptoms and affective disturbances.
3] Structural and Functional Brain Abnormalities:
a) Grey Matter Reductions: Studies have consistently shown decreased grey matter volume in various brain regions, including the prefrontal cortex, hippocampus, and temporal lobe, in individuals with schizophrenia.
b) White Matter Abnormalities: Disruptions in white matter, which connect different brain regions, have also been observed, potentially affecting information processing and communication.
c) Hypofrontality: Reduced activity in the prefrontal cortex, a region involved in executive functions, has been implicated in the cognitive impairments associated with schizophrenia.
4. Neurodevelopmental Factors:
a) Prenatal and Perinatal Influences: Exposure to various prenatal and perinatal factors, such as infections, malnutrition, and complications during childbirth, have been linked to increased risk for schizophrenia.
b) Abnormal Brain Development: These factors may disrupt the normal development of brain structures and circuitry, leading to vulnerability to the disorder.
Diagnosis of Schizophrenia:
a) Clinical interview: A detailed discussion with a mental health professional to gather information about the individual’s symptoms, medical history, family history, and social functioning.
b) Mental status examination: An assessment of the individual’s cognitive functions, mood, and behavior.
c) Neurological examination: A physical examination to rule out other medical conditions that could cause similar symptoms.
d) Psychological testing: Standardized tests to assess cognitive functions, personality, and emotional state.
e) Medical history review: A review of the individual’s medical records to identify any underlying medical conditions.
f) Family history assessment: A review of the individual’s family history to determine if there is a family history of mental illness.
Treatment of Schizophrenia:
A] Pharmacological Treatment -
Antipsychotic medications are the cornerstone of schizophrenia treatment. These drugs help to reduce psychotic symptoms such as hallucinations, delusions, and disorganized thoughts. They are classified into two main categories: typical antipsychotics and atypical antipsychotics.
i) Typical Antipsychotics: These older medications, such as chlorpromazine and haloperidol, primarily target dopamine receptors in the brain. While effective in reducing positive symptoms, they can often cause significant side effects, including motor disturbances like tremors, rigidity, and tardive dyskinesia.
ii) Atypical Antipsychotics: Newer medications, such as clozapine, risperidone, and olanzapine, have a broader range of targets in the brain, including serotonin Receptors. They are generally better tolerated than typical antipsychotics and can be more effective in treating negative symptoms, such as social withdrawal and lack of motivation.
B] Psychotherapy -
Psychotherapy plays a crucial role in schizophrenia treatment, helping patients to develop coping skills, improve social functioning, and enhance overall quality of life.
i) Cognitive-Behavioral Therapy (CBT): CBT focuses on identifying and
challenging negative thoughts and beliefs that contribute to psychotic symptoms. It helps patients to develop healthier coping mechanisms and improve their ability to manage stress.
ii) Family Therapy: Family therapy involves educating family members about
schizophrenia and providing support and guidance. It can help to reduce stress and improve communication within the family.
iii) Social Skills Training: Social skills training helps patients to develop the interpersonal skills necessary for successful social interactions. This can involve role-playing exercises, assertiveness training, and problem-solving techniques.
Long-acting injectable medications:-
Several long-acting injectable antipsychotics are available, each with its unique characteristics and dosing requirements. Some of the most commonly used long-acting injectable medications include:
I] Aripiprazole:
Aripiprazole is a dopamine partial agonist and serotonin antagonist which used in the treatment of schizophrenia. Its long-acting injectable (LAI) formulations offer significant advantages for patients with schizophrenia, particularly those who struggle with medication adherence.
Mechanism of Action of Aripiprazole -
Aripiprazole’s mechanism of action involves a complex interaction with dopamine and serotonin receptors in the brain. It primarily acts as a partial agonist at dopamine D2 receptors, which are implicated in the symptoms of schizophrenia.
By partially activating these receptors, aripiprazole helps to normalize dopamine neurotransmission, reducing the excessive activity associated with psychotic symptoms.
In addition to its effects on dopamine receptors, aripiprazole also antagonizes serotonin 5-HT1A receptors. This interaction is believed to contribute to the medication’s antipsychotic effects and may also help to improve mood and reduce negative symptoms of schizophrenia.
Side Effects:
Movement disorders, Weight gain, Sleepiness, Increased cholesterol, Headache, Injection site reactions
II] Risperidone:
Risperidone is a second-generation antipsychotic medication available in both oral and long-acting injectable (LAI) formulations. The LAI form is specifically Risperdal Consta and is designed to provide sustained release of the medication over several weeks or months, making it a valuable option for individuals with schizophrenia who struggle with medication adherence.
Mechanism of Action -
Risperidone exerts its therapeutic effects primarily by blocking receptors for dopamine and serotonin in the brain. Dopamine is a neurotransmitter implicated in the positive symptoms of schizophrenia, such as hallucinations and delusions, while serotonin plays a role in mood regulation and negative symptoms, like
apathy and social withdrawal. By modulating these neurotransmitter systems, risperidone helps to reduce psychotic symptoms and improve overall functioning.
Side Effects -
Weight Gain, Sedation, Fluctuations in Hormone Levels, Obesity, High Blood Pressure, High Blood Sugar, and Abnormal Cholesterol Levels.
III] Olanzapine:
Olanzapine, when administered as a long-acting injectable (LAI), is a medication used to treat schizophrenia. It offers several advantages over oral formulations.
Mechanism of Action -
Dopamine D2 and Serotonin 5-HT2A receptor antagonism: Olanzapine primarily works by blocking the activity of dopamine D2 and serotonin 5-HT2A receptors in the brain. These receptors are involved in the transmission of neurotransmitters, which play a crucial role in the development of schizophrenia.
Other receptor interactions: In addition to dopamine D2 and serotonin 5-HT2A
receptors, olanzapine also interacts with other receptors, such as histamine H1 and muscarinic M1 receptors. These interactions contribute to some of the medication’s side effects.
Side Effects:
Weight gain, Sedation, tremors, rigidity, restlessness, dry mouth, constipation, blurred vision, urinary retention, and Prolactin elevation.
IV] Paliperidone:
Paliperidone palmitate is a long-acting injectable (LAI) antipsychotic medication used in the treatment of schizophrenia. It is a depot formulation of paliperidone, a second-generation antipsychotic agent.
Mechanism of Action -
Paliperidone is the active metabolite of risperidone and acts primarily as a dopamine D2 receptor antagonist. This receptor antagonism helps to reduce the excessive dopamine activity in the brain that is believed to contribute to the symptoms of schizophrenia. Additionally, paliperidone has an affinity for serotonin 5-HT2A
receptors, which may also play a role in its antipsychotic effects. Side Effects -
Dystonia, Parkinsonism, Weight gain, Increased blood sugar, increased cholesterol, Sedation.
V] Haloperidol:
Haloperidol decanoate is a long-acting injectable formulation of the antipsychotic drug that is widely used in the management of schizophrenia.
Mechanism of Action
Haloperidol, a typical antipsychotic, exerts its therapeutic effects primarily by blocking dopamine receptors in the brain. Dopamine is a neurotransmitter involved in the regulation of mood, thought, and movement. By antagonizing dopamine
receptors, haloperidol helps to reduce the positive symptoms of schizophrenia, such as hallucinations and delusions.
Side Effects –
Dystonia, Parkinsonism, Tardive Dyskinesia, Neuroleptic Malignant Syndrome, Weight Gain, Sedation.
Advantages of Long-acting injectables -
1. Improved Adherence:
a) Reduced Missed Doses: LAI medications ensure consistent drug delivery, minimizing the risk of missed doses that can lead to relapse.
b) Enhanced Compliance: For patients with difficulty adhering to oral medication regimens, LAI can be a more effective treatment option.
2. Sustained Therapeutic Levels:
a) Consistent Efficacy: LAI risperidone maintains steady therapeutic levels of the medication, providing consistent symptom control.
b) Reduced Fluctuations: Unlike oral formulations, LAI avoids the peaks and troughs associated with daily dosing, leading to more stable clinical outcomes.
3. Improved Quality of Life:
a) Enhanced Functioning: Consistent symptom management can improve daily functioning and overall quality of life for individuals with schizophrenia.
b) Reduced Hospitalizations: By preventing relapses, LAI can reduce the need for hospitalization, which can be disruptive and costly.
4. Convenience:
a) Less Frequent Administration: LAI risperidone is typically administered every two weeks or monthly, reducing the burden of daily medication management.
b) Increased Autonomy: For patients who struggle with self-medication, LAI can empower them to take control of their treatment.
5. Cost-Effectiveness:
a) Reduced Relapse Rates: By improving adherence and reducing relapse, LAI can lead to long-term cost savings due to fewer hospitalizations and treatment
interventions.
b) Improved Outcomes: LAI can result in better overall outcomes, potentially reducing the need for additional treatments or services.
REFERENCE
- Stahl SM, Morrissette DA, Citrome L, et al. “Meta-guidelines” for the management of patients with schizophrenia. CNS Spectr. 2013;18(3):150–162.
- Siever LJ, Davis KL. The pathophysiology of schizophrenia disorders: perspectives from the spectrum. Am J Psychiatry. 2004;161(3):398–413.
- Van Os J, Kapur S. Schizophrenia. Lancet. 2009;374(9690):635–645.
- Kishimoto T, Robenzadeh A, Leucht C, et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of Randomized trials. Schizophr Bull. 2014;40(1):192–213.
- Kane J, Honigfeld G, Singer J, et al. Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45(9):789–796.
- Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209– 1223.
- Meltzer L, Li Z, Kaneda Y, Ichikawa J. Serotonin receptors: their key role in drugs to treat schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry.2003;27(7):1159–1172.
- Silverman JM, Siever LJ, Horvath TB, Coccaro EF, Klar H, Davidson M, Pinkham L, Apter SH, Mohs RC, Davis KL: Schizophrenia related and affective personality disorder traits in relatives of Probands with schizophrenia and personality disorders. Am J Psychiatry 1993; 150:435–442.
- Battaglia M, Bernardeschi L, Franchini L, Bellodi L, Smeraldi E: A family study of schizotypal disorder. Schizophr Bull 1995; 21: 33–45.
- Kendler KS, Ochs AL, Gorman AM: The structure of schizotypy: A pilot multitrait twin study. Psychiatry Res 1991; 36:19–36.
- Fanous A, Gardner C, Walsh D, Kendler KS: Relationship between positive and negative symptoms of schizophrenia and Schizotypal symptoms in nonpsychotic relatives. Arch Gen Psy-Chiatry 2001; 58:669–673.
- Kendler KS, Gruenberg AM, Tsuang MT: Psychiatric illness in First-degree relatives of schizophrenic and surgical control patients: a family study using DSM- III criteria. Arch Gen Psychiatry 1985; 42:770–779.
- Braff DL, Freedman R: Endophenotypes in studies of the genetics of schizophrenia, in Neuropsychopharmacology: The Fifth Generation of Progress. Edited by Davis KL, Charney D, Coyle JT, Nemeroff C. Philadelphia, Lippincott Williams & Wilkins, 2002, Pp 703–716.
- Heston LL, Denney D. Interaction between early life experience and biological factors in Schizophrenia. In: The transmission of schizophrenia. Eds Rosenthal D & Kety SS. Oxford Pergamon Press, 1968.
- Higgins J. Effects of child rearing by schizophrenic mothers: a follow-up. Journal of Psychiatric Research, 1976; 13: 1-10.
- Kety SS, Rosenthal D, Wender PH, Schulsinger F. Mental illness in the biological and Adoptive families of adopted schizophrenics. American Journal of Psychiatry, 1971; 128: 302-306.
- Kety SS, Wender PH, Jacobsen B, Ingraham LJ, Janson L, Faber B, Kinney DK. Mental Illness in the biological and adoptive relatives of schizophrenic adoptees. Replication of the Copenhagen study in the rest of Denmark. Archives General Psychiatry, 1994; 51, (6): 442- 455.


 Pruthviraj Awate*
Pruthviraj Awate*


 10.5281/zenodo.14185315
10.5281/zenodo.14185315