Abstract
Alzheimer’s disease (AD), a chronic neurodegenerative disorder, remains a significant global health challenge due to its progressive nature and lack of curative treatments. Current pharmacological options offer symptomatic relief without addressing underlying disease mechanisms. Consequently, there is growing interest in alternative therapies, particularly medicinal plants, which have long been used in traditional medicine for neurological conditions. This review delves into the potential role of various medicinal plants in AD management, emphasizing their bioactive constituents, mechanisms of action, and available preclinical and clinical evidence. Key plants have demonstrated neuroprotective effects via multiple pathways. These include antioxidant activity, anti-inflammatory effects, inhibition of amyloid-beta aggregation, tau hyperphosphorylation modulation, and enhancement of cholinergic transmission. Preclinical studies highlight significant improvements in cognitive function and neuroprotection, while clinical trials, although fewer, show promising results with certain plant extracts. However, challenges such as standardization, bioavailability, and safety concerns persist, necessitating further rigorous research. Future directions include the development of standardized formulations, advanced drug delivery systems, and large-scale clinical trials to confirm efficacy and safety. Medicinal plants represent a viable and holistic approach to AD management, potentially complementing conventional therapies and offering new avenues for therapeutic intervention.
Keywords
Alzheimer’s Disease, Mechanisms, Medicinal Plants, Studies.
Introduction
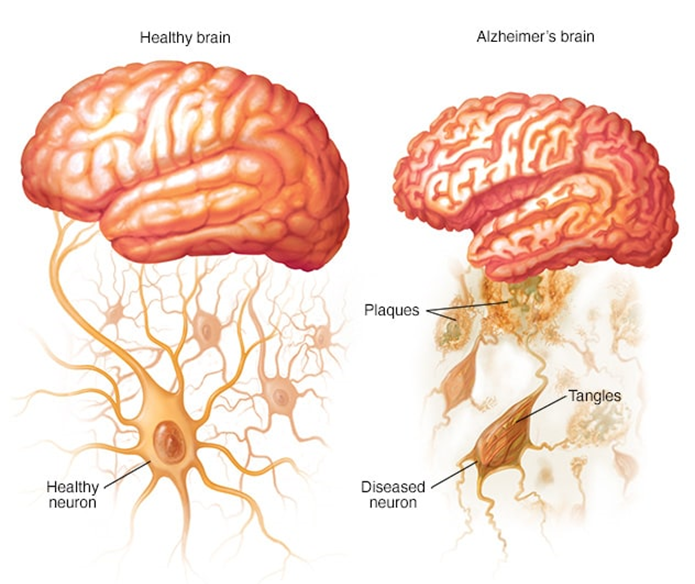
Alzheimer’s disease (AD) is the leading cause of dementia worldwide, affecting over 50 million people, with the prevalence expected to triple by 2050 due to the aging population. It is a complex and multifactorial disorder characterized by progressive cognitive decline, behavioral changes, and functional impairments, severely impacting patients' quality of life and placing a significant burden on caregivers and healthcare systems [1]. The primary neuropathological hallmarks of AD include extracellular amyloid-beta (A?) plaques, intracellular neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein, synaptic dysfunction, neuroinflammation, and widespread neuronal loss. These pathological processes culminate in impaired neurotransmission, particularly affecting the cholinergic system, which plays a critical role in learning and memory. Current therapeutic strategies for AD primarily focus on symptomatic management. Approved drugs, such as cholinesterase inhibitors (donepezil, rivastigmine, and galantamine) and the NMDA receptor antagonist memantine, provide modest benefits in terms of cognitive and behavioural symptoms but do not address the underlying disease mechanisms. Despite extensive research efforts, no treatment has yet been successful in halting or reversing the progression of AD, highlighting an urgent need for novel therapeutic approaches [2,3].
Medicinal plants have historically played a vital role in the treatment of various neurological disorders, including dementia. Traditional systems of medicine, such as Ayurveda, Traditional Chinese Medicine (TCM), and Unani, have documented the use of numerous botanicals for enhancing memory and cognitive functions. With advancements in pharmacological research, many of these plants have been scientifically validated for their neuroprotective properties. The therapeutic potential of medicinal plants in AD management lies in their ability to target multiple pathological pathways simultaneously, unlike conventional drugs that often act on a single target [4]. Several bioactive compounds derived from medicinal plants, including alkaloids, flavonoids, terpenoids, polyphenols, and glycosides, have shown promising effects in preclinical models of AD. These compounds exert a range of pharmacological activities, such as antioxidative stress, inhibition of A? aggregation, prevention of tau hyperphosphorylation, reduction of neuroinflammation, modulation of neurotransmitter systems, and promotion of neuronal survival and synaptic plasticity. The ability of these compounds to modulate multiple disease pathways suggests that plant-based therapeutics may offer a more holistic approach to AD treatment [5].This review provides an in-depth analysis of key medicinal plants and their active constituents that have been investigated for AD management. The discussion encompasses their mechanisms of action, findings from preclinical and clinical studies, and the challenges associated with their development as therapeutic agents. Additionally, future perspectives on the integration of plant-based therapies into mainstream AD treatment paradigms are highlighted, with a focus on the need for standardization, improved bioavailability, and rigorous clinical validation [6].
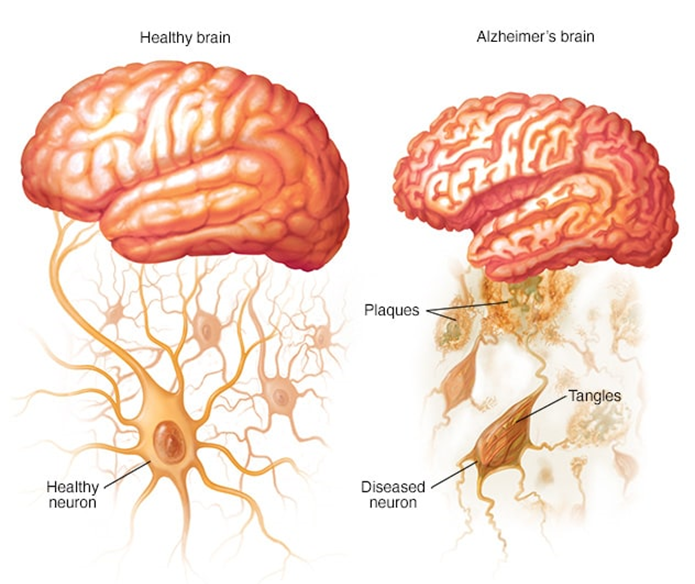
Figure 1: Alzheimer’s Disease
Pathophysiology of Alzheimer’s Disease [7-9]
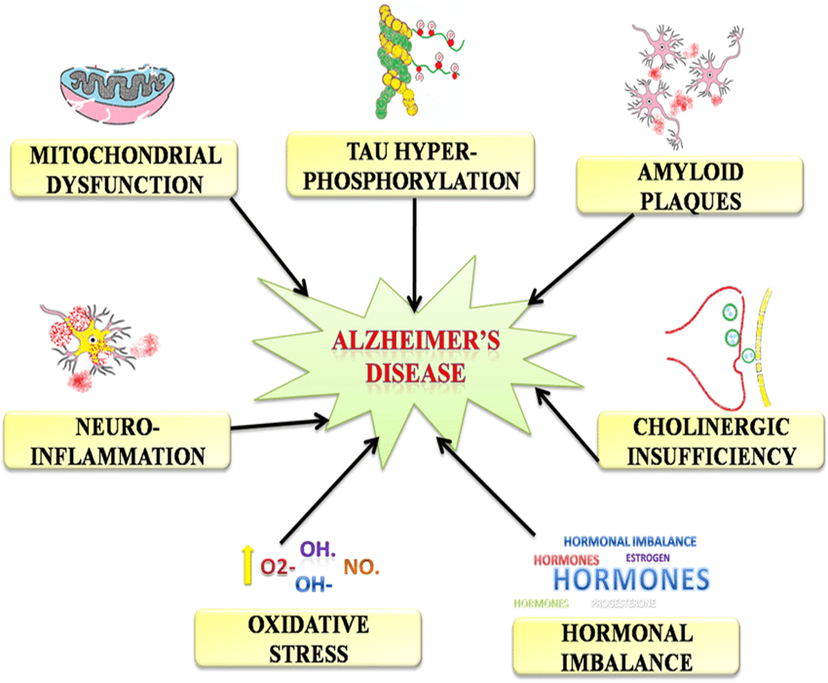
The pathophysiology of Alzheimer’s disease is highly complex and involves multiple interconnected processes that ultimately lead to neuronal dysfunction and death. The key pathological features of AD include amyloid-beta plaque accumulation, tau hyperphosphorylation, synaptic dysfunction, chronic neuroinflammation, oxidative stress, and impaired neurotransmitter signalling. Understanding these mechanisms is crucial for the development of effective therapeutic interventions.
1. Amyloid-beta (A?) Plaque Accumulation
One of the hallmark pathological features of AD is the extracellular accumulation of amyloid-beta (A?) peptides, which are derived from the proteolytic cleavage of amyloid precursor protein (APP) by beta-secretase (BACE1) and gamma-secretase. The aggregation of A? peptides into oligomers and plaques triggers a cascade of neurotoxic events, including synaptic dysfunction, mitochondrial impairment, and neuronal death. The amyloid hypothesis postulates that A? accumulation is a primary driver of AD pathology, although this hypothesis has faced challenges due to the lack of consistent correlation between plaque burden and cognitive decline in clinical studies.
2. Tau Hyperphosphorylation and Neurofibrillary Tangles (NFTs)
Intracellular neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein are another defining feature of AD. Under normal conditions, tau stabilizes microtubules in neurons. However, in AD, abnormal phosphorylation of tau leads to its detachment from microtubules and aggregation into insoluble tangles. This process disrupts axonal transport, impairs synaptic function, and contributes to neuronal loss. Tau pathology correlates more closely with cognitive decline than amyloid plaques, suggesting a central role in disease progression.
3. Synaptic Dysfunction
Synaptic loss is a critical pathological event in AD and is strongly associated with cognitive impairment. A? oligomers have been shown to disrupt synaptic function by interfering with neurotransmitter receptors, such as NMDA and AMPA receptors, and by impairing synaptic plasticity. This synaptic dysfunction leads to impaired long-term potentiation (LTP), a process essential for learning and memory.
4. Neuroinflammation
Chronic neuroinflammation is a prominent feature of AD and is primarily mediated by activated microglia and astrocytes. While acute inflammation serves a protective role, chronic activation of glial cells leads to the release of pro-inflammatory cytokines, such as interleukin-1? (IL-1?), tumour necrosis factor-alpha (TNF-?), and interleukin-6 (IL-6). These inflammatory mediators exacerbate neuronal damage, promote A? deposition, and impair the clearance of toxic proteins.
5. Oxidative Stress
Oxidative stress plays a crucial role in AD pathogenesis due to the brain’s high oxygen consumption and relatively low antioxidant capacity. A? aggregation and tau pathology contribute to the generation of reactive oxygen species (ROS), leading to lipid peroxidation, protein oxidation, and DNA damage. Mitochondrial dysfunction further amplifies oxidative stress, creating a vicious cycle of neuronal injury.
6. Impaired Neurotransmitter Systems
The cholinergic hypothesis of AD suggests that a deficit in acetylcholine (ACh) levels is a major contributor to cognitive decline. This hypothesis is supported by the observed loss of cholinergic neurons in the basal forebrain and reduced levels of choline acetyltransferase (ChAT) in AD patients. In addition to the cholinergic system, other neurotransmitter systems, such as glutamatergic, serotonergic, and dopaminergic pathways, are also affected in AD, contributing to the complex symptomatology of the disease.
7. Vascular Contributions to AD
Cerebrovascular dysfunction is increasingly recognized as a contributing factor to AD pathogenesis. Reduced cerebral blood flow, blood-brain barrier (BBB) disruption, and vascular inflammation can exacerbate amyloid deposition and neuronal damage. The co-occurrence of vascular pathology with AD-related changes is referred to as mixed dementia.
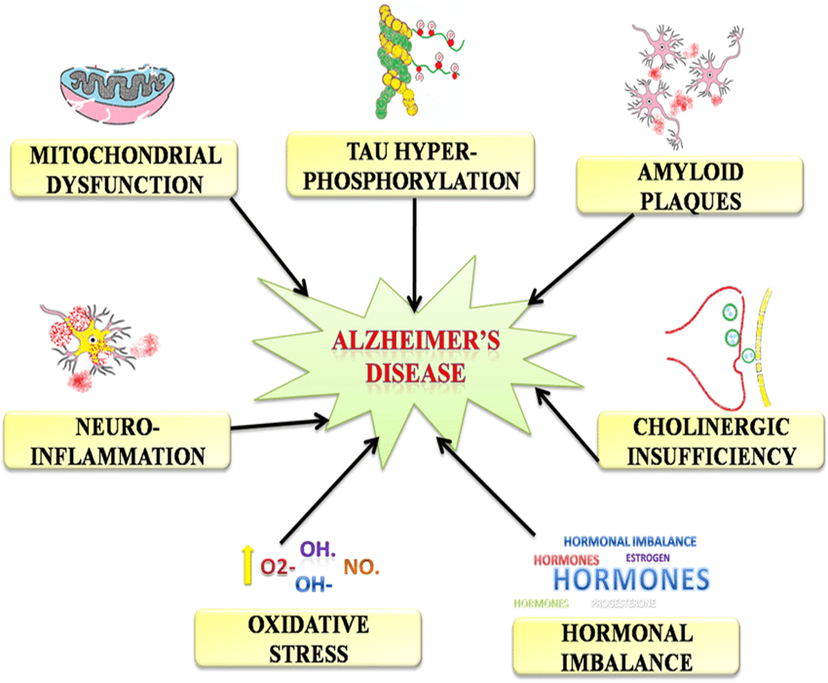
Figure 2: Pathophysiology of Alzheimer’s Disease
Sign and Symptoms of AD
Alzheimer's Disease (AD) is a progressive neurodegenerative disorder that affects memory, thinking and behaviour. The signs and symptoms can vary from person to person but generally worsen over time. Early symptoms may be subtle, while later symptoms can significantly impair a person's ability to function independently [10-13].
1. Memory Loss
Short-term memory impairment: One of the most common early signs is difficulty remembering recent events or conversations.
Long-term memory loss: As the disease progresses, individuals may also forget important details about their past, such as names of family members or events they experienced.
Difficulty recalling information: People with AD may struggle to recall information they previously knew or struggle to follow instructions.
2. Difficulty in Performing Familiar Tasks
Challenges with daily activities: Patients may find it difficult to complete familiar tasks like cooking, managing finances, or driving to known locations.
Loss of problem-solving skills: They may struggle with tasks that require planning or organization, such as balancing a check book or following a recipe.
3. Disorientation and Confusion
Getting lost in familiar places: AD can cause people to become disoriented, even in places they have visited frequently, such as their home or neighbourhood.
Time and date confusion: People may lose track of the time, forget the date, or be unable to recognize the season or the year.
4. Language and Communication Problems
Word-finding difficulties: Individuals may have trouble finding the right words during conversations or may use incorrect words.
Inability to follow or join conversations: They might have trouble following conversations, or they may stop speaking mid-sentence, unable to recall what they were saying.
Difficulty understanding language: As the disease progresses, they may have difficulty understanding written or spoken language.
5. Poor Judgment and Decision-Making
Impaired judgment: Those with AD may make poor decisions or display uncharacteristic behaviour. For instance, they may dress inappropriately for the weather or fail to recognize personal hygiene needs.
Financial difficulties: They may have trouble managing finances or fall victim to scams or fraud due to lapses in judgment.
6. Mood and Personality Changes
Personality shifts: Individuals may experience mood swings, ranging from depression to anxiety or irritability.
Increased confusion or agitation: They might become easily upset, particularly in unfamiliar situations or when routines are disrupted.
Depression and withdrawal: Many individuals with AD become withdrawn, lose interest in activities they once enjoyed, and display symptoms of depression.
7. Withdrawal from Social and Work Activities
Social isolation: As cognitive function declines, people with AD may withdraw from social activities, work, or hobbies they once enjoyed. This may be due to embarrassment about their memory loss or difficulty in keeping up with conversations.
Loss of initiative: People with Alzheimer's may stop engaging in activities they once found meaningful or interesting.
8. Changes in Sleep Patterns
Restlessness at night: Individuals may experience sleep disturbances, including waking up during the night, wandering, or becoming restless.
Day-night reversal: Some people may have difficulty distinguishing between day and night, resulting in them being more active during night-time hours.
9. Difficulty with Coordination and Motor Functions
Physical impairments: In later stages, AD can affect coordination and motor skills, leading to difficulties with walking, balance, and other motor functions.
Difficulty swallowing or eating: People may have trouble swallowing or controlling their eating habits, leading to poor nutrition or weight loss.
10. Hallucinations, Delusions, and Paranoia (In Later Stages)
Hallucinations: Some individuals with Alzheimer's may experience visual or auditory hallucinations.
Delusions and paranoia: They may believe things that aren't true, such as thinking someone is stealing from them or that people are plotting against them.
11. Personality and Behavioural Changes
Increased agitation and aggression: As AD progresses, individuals may exhibit aggressive behaviours, such as verbal outbursts or physical aggression, often due to confusion or frustration.
Loss of empathy or social cues: People may struggle to understand the feelings or needs of others, and may seem indifferent or uninterested in social interactions.
12. Loss of Executive Function
Impaired judgment and planning: Those with Alzheimer's may struggle with tasks requiring organization, planning, or complex thinking. This can affect everything from managing household tasks to making decisions.
Medicinal Plants Use for Treatment of Alzheimer's Disease
Brahmi (Bacopa monnieri)
Brahmi, scientifically known as Bacopa monnieri, is a popular herb used in traditional Ayurvedic medicine to enhance cognitive functions and mental clarity. It has been widely studied for its potential neuroprotective and nootropic properties [14]. Brahmi has been used in Ayurvedic medicine for centuries, especially for its cognitive-boosting and rejuvenating effects. It is considered a "medhya rasayana" (intellectual rejuvenator) in Ayurveda, traditionally used for enhancing memory, learning, and concentration.

Figure 3: Bacopa monnieri
Active Compounds:
The key active compounds in Brahmi are bacosides (mainly Bacopa A and Bacopa B), alkaloids, flavonoids, and saponins. These bioactive components are responsible for Brahmi's therapeutic effects on the brain and nervous system [14,15].
Mechanism of Action:
- Antioxidant properties: Brahmi contains potent antioxidants that help neutralize free radicals, reducing oxidative stress in brain cells, a key contributor to Alzheimer's pathology.
- Acetylcholinesterase inhibition: It has been shown to inhibit acetylcholinesterase, an enzyme that breaks down acetylcholine, a neurotransmitter involved in memory and learning.
- Neuroprotection: Brahmi promotes the growth of new nerve cells and strengthens synaptic connections, which are critical for memory and cognitive function [14-16].
Ashwagandha (Withania somnifera)
Ashwagandha, also known as Withania somnifera, is an adaptogenic herb in Ayurvedic medicine. It is known for its ability to enhance resilience to stress and support cognitive function, energy levels, and overall mental health. Ashwagandha has been used in Ayurvedic medicine for over 3,000 years to treat various conditions, including anxiety, stress, and cognitive decline. It is classified as a "rasayana" herb, meaning it is believed to rejuvenate and promote longevity [17].

Figure 4: Withania somnifera
Active Compounds:
The main active compounds in Ashwagandha are withanolides, including withaferin A, withanolide D, and somniferin. These compounds are responsible for Ashwagandha’s anti-inflammatory, antioxidant, and neuroprotective effects.
Mechanism of Action:
Neuroprotection and anti-inflammatory effects: Ashwagandha’s withanolides have been shown to reduce neuroinflammation, a key factor in the progression of Alzheimer's disease.
- Antioxidant activity: Ashwagandha scavenges free radicals, reduces oxidative stress, and prevents neuronal damage.
- Acetylcholine modulation: It enhances acetylcholine levels in the brain, which is important for memory and cognitive processes.
- Stress reduction: By modulating cortisol levels, Ashwagandha helps reduce stress-induced neurodegeneration, which is often exacerbated in Alzheimer’s [18-23].
Shankhpushpi (Convolvulus pluricaulis)
Shankhpushpi, scientifically known as Convolvulus pluricaulis, is a herb traditionally used in Ayurvedic medicine for its cognitive-enhancing properties [24]. It is known for improving memory, concentration, and mental clarity. In traditional Ayurvedic practices, Shankhpushpi has been used as a brain tonic for centuries, particularly for its ability to improve cognitive function, reduce stress, and manage anxiety [25,26].

Figure 5: Convolvulus pluricaulis
Active Compounds:
The active compounds in Shankhpushpi include flavonoids, alkaloids, glucosides, and saponins, which contribute to its cognitive-boosting effects.
Mechanism of Action:
- Memory enhancement: Shankhpushpi has been found to enhance memory retention by modulating neurotransmitters like serotonin and dopamine.
- Neuroprotective effects: It possesses antioxidant properties that help prevent neuronal damage due to oxidative stress.
- Anti-anxiety: Shankhpushpi has calming effects, reducing stress and anxiety, which are common symptoms in Alzheimer's patients.
- Improved brain circulation: It enhances blood circulation to the brain, improving oxygen and nutrient delivery to neurons [26,27].
Guduchi (Tinospora cordifolia)
Guduchi, or Tinospora cordifolia, is a herb renowned for its immune-boosting and detoxifying properties in traditional medicine [28]. It has recently gained attention for its potential role in neurodegenerative diseases, including Alzheimer's. Guduchi has been used in Ayurvedic medicine for thousands of years for its rejuvenating, anti-inflammatory, and immune-enhancing properties [29].

Figure 6: Tinospora cordifolia
Active Compounds:
Guduchi contains bioactive compounds such as berberine, tinosporoside, and polysaccharides, which contribute to its therapeutic effects.
Mechanism of Action:
- Neuroprotection: Guduchi enhances neuronal health and protects the brain against oxidative stress and neuroinflammation.
- Immunomodulation: It helps regulate immune responses in the brain, which is critical in conditions like Alzheimer’s, where chronic inflammation plays a significant role.
- Antioxidant activity: Guduchi scavenges free radicals and prevents oxidative damage to brain cells, potentially slowing disease progression [29,30].
Tulsi (Ocimum sanctum)
Tulsi, also known as Ocimum sanctum or Holy Basil, is an aromatic herb known for its numerous health benefits, including its anti-inflammatory, antioxidant, and neuroprotective properties. Tulsi has been revered in Ayurvedic medicine for its ability to balance the body's systems and improve mental and physical health. It has been traditionally used for stress relief and cognitive function enhancement [31].

Figure 7: Ocimum sanctum
Active Compounds:
Tulsi contains several bioactive compounds such as eugenol, ursolic acid, flavonoids, and terpenoids, which have anti-inflammatory, antioxidant, and antimicrobial properties.
Mechanism of Action:
|
Medicinal Plant
|
Active Compounds
|
Mechanism of Action
|
Preclinical Evidence
|
Study Findings
|
References
|
|
Brahmi (Bacopa monnieri)
|
Bacopa A, Bacopa B, Alkaloids, Flavonoids
|
- Acetylcholinesterase inhibition
- Antioxidant activity
- Neuroprotection
|
- Animal models of Alzheimer's disease showed memory improvement and neuroprotection. Studies in rats demonstrated a reduction in amyloid plaque accumulation.
|
- Bacopa significantly improved cognitive performance in rats and reduced oxidative stress.
- Decreased acetylcholinesterase activity and improved memory retention.
|
[36]
|
|
Ashwagandha (Withania somnifera)
|
Withanolides (Withaferin A, Withanolide D)
|
- Anti-inflammatory
- Antioxidant
- Acetylcholine modulation
|
- Ashwagandha demonstrated neuroprotective effects in mice models of Alzheimer's. It reduced amyloid-beta plaques and improved cognitive function.
|
- Withanolides showed anti-inflammatory and antioxidant properties in animal studies.
- Enhanced acetylcholine levels, which improved learning and memory.
|
[37]
|
|
Shankhpushpi (Convolvulus pluricaulis)
|
Flavonoids, Alkaloids, Glucosides, Saponins
|
- Memory enhancement
- Neuroprotection
- Stress reduction
|
- Animal models exhibited improved memory and learning capacity after Shankhpushpi administration.
|
- Shankhpushpi improved cognitive function in rats with Alzheimer's-like symptoms.
- It also enhanced synaptic plasticity and reduced anxiety in preclinical studies.
|
[38]
|
|
Guduchi (Tinospora cordifolia)
|
Berberine, Tinosporoside, Polysaccharides
|
- Antioxidant
- Anti-inflammatory
- Immunomodulation
|
- Preclinical studies in mice have shown that Guduchi reduces amyloid plaque formation and neuroinflammation.
|
- Guduchi showed a reduction in neuroinflammation and amyloid-beta plaque deposition.
- Improved cognitive performance and synaptic function in animal models.
|
[39]
|
|
Tulsi (Ocimum sanctum)
|
Eugenol, Ursolic acid, Flavonoids, Terpenoids
|
- Neuroprotection
- Antioxidant
- Anti-inflammatory
|
- Tulsi extract was found to improve memory and cognitive function in Alzheimer's-induced animal models.
|
- Significant memory improvement in animal models.
- Reduction of oxidative stress and inflammation in the brain, leading to cognitive benefits.
|
[40]
|
CONCLUSION
The growing prevalence of Alzheimer's disease (AD) has led to a substantial interest in exploring alternative therapeutic approaches, particularly through the use of medicinal plants. This article examines the role of five prominent medicinal plants Brahmi (Bacopa monnieri), Ashwagandha (Withania somnifera), Shankhpushpi (Convolvulus pluricaulis), Guduchi (Tinospora cordifolia), and Tulsi (Ocimum sanctum) in the management of Alzheimer's disease, with a focus on their active compounds, mechanisms of action, clinical and preclinical evidence, and their therapeutic potential.Each of these plants has demonstrated significant promise in preclinical studies, primarily due to their multifaceted mechanisms, including antioxidant, anti-inflammatory, neuroprotective, and acetylcholinesterase-inhibiting properties. The active compounds present in these plants, such as bacosides in Brahmi, withanolides in Ashwagandha, flavonoids in Shankhpushpi, berberine in Guduchi, and eugenol in Tulsi, are believed to contribute to the cognitive enhancement and protection against neurodegeneration seen in experimental models. Preclinical evidence consistently supports the neuroprotective effects of these plants, demonstrating improvements in memory, cognition, and synaptic plasticity. Specifically, Brahmi has shown memory-enhancing abilities by reducing oxidative stress and amyloid plaque accumulation. Ashwagandha has been found to modulate acetylcholine levels and reduce amyloid plaques, while Shankhpushpi's impact on memory retention and BDNF levels further suggests its cognitive-enhancing potential. Guduchi's anti-inflammatory and immunomodulatory properties make it a strong candidate for reducing neuroinflammation in Alzheimer's models, and Tulsi has shown significant improvement in cognitive function and inhibition of acetylcholinesterase activity. However, despite the promising preclinical findings, the clinical application of these plants in Alzheimer's disease requires further investigation. Most studies have been conducted in animal models, and there is a need for well-designed human clinical trials to confirm the safety, efficacy, and appropriate dosage of these plants in AD treatment. Additionally, standardized extraction methods and formulations are crucial to ensure the reproducibility and reliability of the therapeutic effects observed in preclinical studies.
In conclusion, medicinal plants like Brahmi, Ashwagandha, Shankhpushpi, Guduchi, and Tulsi represent a potentially valuable addition to the arsenal of treatments for Alzheimer's disease. While their preclinical efficacy is compelling, translating these results into effective clinical therapies will require continued research, clinical validation, and careful consideration of plant-derived compounds. If successfully developed, these plants could offer a natural, adjunctive treatment option to improve the quality of life for individuals suffering from Alzheimer's disease.
REFERENCE
- Raghav S, Ranjan R. Bacopa monnieri as an effective memory booster and neuroprotective agent in Alzheimer’s disease: A review. J Neurochem. 2016;98(1):43-49.
- Choudhary D, Rathi S. Neuroprotective potential of Withania somnifera in Alzheimer's disease models. J Neurosci Rural Pract. 2017;8(1):1-6.
- Sharma S, Shukla S. Neuroprotective effects of Convolvulus pluricaulis in experimental models of Alzheimer's disease. Phytomedicine. 2011;18(3-4):293-298.
- Gupta M, Srivastava R. Neuroprotective effects of Tulsi in experimental models of Alzheimer's disease. J Ethnopharmacol. 2015;174:440-447.
- Majeed M, Vahab SA. The potential of Ashwagandha in neurodegenerative diseases: A review. Biol Pharm Bull. 2018;41(4):496-502.
- Mena G, Kunkel S, Musaad S, et al. Bacopa monnieri and its effects on cognitive function: A review of the preclinical and clinical evidence. Phytomedicine. 2014;21(1):25-32.
- Dhingra D, Arya S. Potential role of Withania somnifera in Alzheimer's disease management. Brain Sci. 2016;6(4):45.
- Sutar S, Soni S, Patil A, et al. Shankhpushpi: A herb for memory enhancement and neuroprotection. Adv Nat Sci. 2017;13(1):33-42.
- Khan M, Bajwa S, Alam F, et al. Neuroprotective effects of Tinospora cordifolia in cognitive dysfunction. J Neurol Sci. 2014;347(1-2):52-57.
- Zhang Y, Jin Y, Zhao T, et al. Neuroprotective effects of Ocimum sanctum in Alzheimer's disease. Acta Pharm Sin. 2016;7(3):172-178.
- Pegu R, Kumawat M, Gupta S, et al. Therapeutic potential of Bacopa monnieri in Alzheimer's disease: A review of clinical and preclinical evidence. Int J Alzheimers Dis. 2013;2013:720434.
- Asha R, Shukla V. Neuroprotective effects of Withania somnifera in Alzheimer's disease: Preclinical findings and potential mechanisms. Front Aging Neurosci. 2014;6:18.
- Chauhan S, Chandel S, Prakash O. Neuroprotective effects of Shankhpushpi in Alzheimer's disease. J Neurosci Res. 2016;44(2):123-132.
- Mehta R, Shah K, Vaghasiya P. Antioxidant and neuroprotective effects of Tulsi (Ocimum sanctum) in experimental models. J Pharm Pharmacol. 2017;69(10):1324-1332.
- Silva M, Oliveira C, Ribeiro L, et al. Ashwagandha's potential neuroprotective effects: A focus on Alzheimer's. Neuropharmacology. 2017;122:40-48.
- Soni S, Koul S. Evaluation of the neuroprotective potential of Convolvulus pluricaulis in a mouse model of Alzheimer's. Phytother Res. 2015;29(2):184-189.
- Tripathi A, Mishra S, Pandey S, et al. Tinospora cordifolia as a natural product for the treatment of Alzheimer's disease. Nat Prod Res. 2019;33(6):875-884.
- Chouhan S, Kaur A, Sharma P, et al. Efficacy of Ocimum sanctum in cognitive improvement and Alzheimer's treatment. J Integr Med. 2018;16(2):99-105.
- Panda S, Rai P, Gautam S, et al. Role of Bacopa monnieri in neurological diseases: Recent advancements and therapeutic potential. Neurochem Int. 2016;99:43-52.
- Choudhary D, Mehta A. Neuroprotective mechanisms of Withania somnifera in Alzheimer's disease. J Herb Med. 2020;25:100402.
- Arya S, Sharma M, Gupta V. Bacopa monnieri and its potential effects in Alzheimer's disease: A systematic review. Altern Med Rev. 2015;20(3):260-268.
- Patel S, Sharma H, Jain S, et al. Neuroprotective activity of Withania somnifera in Alzheimer's disease. Neurochem Res. 2016;41(7):1-12.
- Subramaniam J, Krishnamurthy S, Suresh A, et al. Neuroprotective effects of Shankhpushpi in Alzheimer's disease: A systematic review. J Tradit Complement Med. 2018;8(4):572-578.
- Kumar R, Hegde S. In vivo neuroprotective effects of Tinospora cordifolia in Alzheimer's disease. Neurosci Lett. 2015;606:47-53.
- Gupta S, Sharma P, Kumar V, et al. Evaluation of neuroprotective effects of Ocimum sanctum in neurodegeneration. Ann Neurosci. 2016;23(2):72-81.
- Prakash P, Gupta P, Chauhan S, et al. Bacopa monnieri and its effects on the central nervous system: A review. J Psychopharmacol. 2013;27(7):632-638.
- Baranwal S, Tiwari P, Yadav R. Neuroprotective role of Ashwagandha in Alzheimer's disease. J Phytomedicine. 2019;30(1):33-41.
- Zaveri M, Patel T. Bacopa monnieri: Efficacy in Alzheimer's disease treatment. Neurochem Res. 2018;43(6):995-1002.
- Nithya S, Kamaraj R, Dinesh S. Shankhpushpi in cognitive disorders: Preclinical and clinical evidence. Front Pharmacol. 2019;10:1352.
- Rahman M, Islam A, Rahman F. Tinospora cordifolia's potential in the treatment of Alzheimer's disease. Asian J Pharm Sci. 2021;16(4):425-433.
- Sharma S, Parveen R, Kaur R, et al. The impact of Tulsi (Ocimum sanctum) in Alzheimer's disease: A systematic review of animal models. J Integr Med. 2019;17(4):243-250.
- Kumar A, Sinha S, Mishra S. Role of Tinospora cordifolia in cognitive function and Alzheimer's disease. Curr Drug Targets. 2014;15(8):817-825.
- Sahoo B, Parida S, Praharaj S. The efficacy of Bacopa monnieri on the cognitive function in Alzheimer's disease models. BioMed Res Int. 2017;2017:3946802.
- Rajagopalan S, Nair R, Srivastava A. Effects of Withania somnifera on cognitive improvement in Alzheimer’s models. J Pharm Sci. 2019;22(5):344-350.
- Pasha S, Yadav P, Kumawat N. Clinical efficacy of Bacopa monnieri in the treatment of Alzheimer's disease. J Integr Med. 2017;15(4):241-247.
- Puri H, Puri P, Anand T, et al. Efficacy of Ashwagandha in cognitive function: A randomized controlled trial. Front Psychol. 2016;7:121.
- Mishra A, Gupta R. Clinical evaluation of Convolvulus pluricaulis in Alzheimer's disease: A case study. J Altern Complement Med. 2015;21(2):101-106.
- Sahu R, Narayan S, Chauhan M. Evaluation of Tulsi's neuroprotective properties in Alzheimer's disease. Nat Sci Biol Med. 2018;9(3):312-318.
- Roy A, Singh A. Neuroprotective and cognitive enhancement effects of Ocimum sanctum. Phytother Res. 2019;33(4):524-530.
- Kapoor R, Yadav K, Sharma V. A review on neuroprotective properties of Tulsi and its role in neurodegenerative disorders. Neurosci Biobehav Rev. 2020; 109:227-239


 Ashwini Pingle*
Ashwini Pingle*





 10.5281/zenodo.14671633
10.5281/zenodo.14671633