Abstract
BACKGROUND : hotgun pellet injuries to the craniofacial and cervical regions can lead to complex trauma involving vital structures, including the brain, ocular region, and vascular system. OBSERVATIONS : We present a case of a 36-year-old male who sustained a craniofacial shotgun injury, with multiple pellets lodged in critical areas, including the right thalamus, cervical vertebra, and orbit, as well as foreign bodies in the subgaleal and maxillary sinus regions.
the patient was conservatively managed, with a focus on monitoring the intrathalamic pellet and vascular structures while surgically removing foreign bodies from the subgaleal space. CONCLUSION: his case highlights the importance of a multidisciplinary approach and careful monitoring in managing complex craniofacial shotgun pellet injuries, particularly when intracranial and vascular complications are involved.
Keywords
hotgun pellet, injurie, craniofacial, conservatively managed
Introduction
Shotgun injuries to the craniofacial region, especially when multiple pellets are involved, can present a complex clinical challenge. Such injuries may result in significant damage to facial structures, intracranial areas, and vascular systems. This case report highlights a 36-year-old male with craniofacial shotgun pellet injuries, including the presence of multiple foreign bodies, intracranial hemorrhage, and vascular complications, along with an unusual presentation involving a foreign body in close contact with the vertebral artery.
Illustrative Case
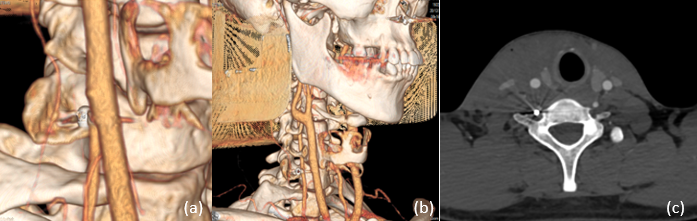
A 36-year-old male patient presented to the emergency department following a shotgun injury to the face and scalp. The patient was fully conscious, hemodynamically stable, and had no signs of respiratory distress. Upon clinical examination, multiple pinpoint facial wounds were noted, along with injuries to the scalp. Ophthalmologic examination revealed no exophthalmos, and ocular mobility was unaffected. However, the patient had abrasions on the lower palpebra and a contusion on the same region of the lower eyelid. A CT scan of the head and neck was performed, revealing a shotgun pellet embedded in the right thalamus, surrounded by a small intraparenchymal hematoma, with slight edema. Multiple foreign bodies were noted in the subgaleal space, and a pellet was located at the left orbital apex, with no damage to the ocular globe. However, significant infiltration of the ipsilateral eyelid was observed. Additionally, a pellet was located in the right transverse foramen of the 7th cervical vertebra, in close contact with the vertebral artery. There were also foreign bodies present along the posterior wall of the maxillary sinus and within the left pharyngeal space. An angioscanner (CT angiography) revealed an unusual small false aneurysm of the right carotid artery, likely resulting from the shotgun pellet’s proximity to the vessel.
The management of this case involved close monitoring and conservative management strategies. Given the presence of the pellet in the right thalamus, it was decided that the patient would be carefully monitored for any signs of neurological deterioration, intracranial pressure changes, or further hemorrhagic complications. The intrathalamic pellet was observed for potential migration or adverse effects, but surgical removal was not initially considered due to its deep and critical location in the thalamus. Simultaneously, the patient’s multiple foreign bodies in the subgaleal space were managed surgically. Foreign body removal was carried out under sterile conditions, focusing on the subgaleal area where the pellets could cause infection or further tissue damage. The pellets located in the facial and scalp regions were extracted to minimize the risk of infection and to prevent further tissue irritation. However, other foreign bodies, particularly those located in the more critical regions . were left in place due to their anatomical location and the risks of surgical intervention. The patient was kept under observation in the intensive care unit (ICU) for 24 hours to monitor for complications, including signs of infection, neurological changes, or vascular events related to the pellet's proximity to the vertebral artery and carotid system. Pain management, along with prophylactic antibiotics, was administered to prevent any infections resulting from the embedded foreign bodies. After the foreign body removal from the subgaleal space, the patient’s condition improved. He remained stable neurologically, with no signs of acute deterioration or complications from the intrathalamic pellet. The false aneurysm of the right carotid artery was monitored carefully through repeat angiography, and no progression or rupture was noted during follow-up. At the six-month follow-up, the patient had made a remarkable recovery. There was no neurological deficit, and the only residual effect was mild facial numbness due to the foreign body removal in the subgaleal region. Imaging confirmed that the foreign bodies in the thalamus, cervical vertebra, and orbital apex had remained stable, without signs of migration or further complications.

Figure.1 CT scan of the head and neck was performed, revealing a shotgun pellet embedded in the right thalamus, surrounded by a small intraparenchymal hematoma, with slight edema. Multiple foreign bodies were noted in the subgaleal space, and a pellet was located at the left orbital apex, with no damage to the ocular globe. However, significant infiltration of the ipsilateral eyelid was observed. Additionally, a pellet was located in the right transverse foramen of the 7th cervical vertebral
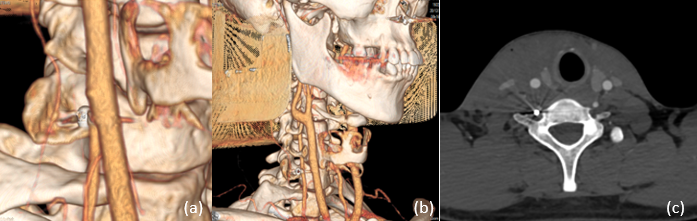
Figure.2. CT angiography) revealed an unusual small false aneurysm of the right carotid artery, likely resulting from the shotgun pellet’s proximity to the vessel.
DISCUSSION
Traumatic injuries caused by shotguns to the craniofacial region present distinct challenges due to the dispersal of multiple pellets, which can lead to a wide range of injuries affecting bone, soft tissues, and vital structures such as blood vessels and the central nervous system. The unique mechanism of injury—dispersed pellets traveling at high velocity—often results in extensive damage that requires immediate attention. Facial trauma due to shotguns can involve fractures of the maxillofacial bones, lacerations, and penetrating wounds, with significant risk for neurological deficits, particularly when the trauma extends to the skull base or intracranial structures [1].
The impact of shotgun injuries is influenced by the range at which the shot is fired. Close-range shots typically cause more severe and widespread damage due to the denser pellet spread, increasing the likelihood of penetrating vital structures. In contrast, long-range shots often lead to less severe damage but can still result in substantial soft tissue injury. In this case, the presence of multiple pellets in various anatomical regions, such as the thalamus and cervical vertebra, highlights the severity and complexity of the injury. The thalamus, being a critical relay center for sensory and motor signals in the brain, is a highly sensitive area to damage. Although thalamic injury in the context of penetrating trauma is rare, it can lead to profound and long-lasting neurological consequences, including sensory loss, motor deficits, and cognitive impairments. The management of thalamic injuries remains challenging due to the difficulty in removing deeply embedded foreign bodies without causing additional neurological damage [2]. In the presented case, the pellet lodged in the right thalamus was managed conservatively due to its deep and critical location. Surgical intervention could have resulted in significant neurological deterioration. Observational management in such cases is commonly preferred unless the pellet causes acute complications, such as progressive hemorrhage or mass effect [3]. One of the more alarming complications in penetrating craniofacial trauma is vascular injury, particularly involving major arteries such as the carotid and vertebral arteries. The proximity of the shotgun pellet to the right carotid artery in this case led to the development of a false aneurysm. Carotid artery pseudoaneurysms are a rare but serious complication of penetrating trauma, often resulting from direct vessel injury due to foreign bodies or bone fragments [4].. False aneurysms may not immediately present symptoms, but they are at risk of rupture, leading to potentially fatal hemorrhage. Management of carotid pseudoaneurysms typically involves close monitoring and, in some cases, surgical intervention, especially if there is evidence of expansion or rupture. In this case, the patient was carefully monitored with repeat angiography, and no signs of rupture or progression of the aneurysm were noted during follow-up, suggesting a stable condition. Conservative management of pseudoaneurysms is acceptable if there is no acute risk of rupture, as it allows for the avoidance of unnecessary surgical risks [5]. The management of foreign bodies embedded in sensitive anatomical regions—such as the thalamus, cervical vertebra, and orbital apex—requires a careful balance between the risks of surgical removal and the potential for long-term complications. As evidenced in this case, foreign bodies located in critical areas like the thalamus and vertebra were left in place to avoid additional neurological or vascular damage, while those in less critical regions, such as the subgaleal space, were surgically removed to reduce the risk of infection and further soft tissue damage [6]. While foreign body removal is generally recommended to prevent infection, migration, and tissue irritation, it must be approached with caution in areas where surgery poses substantial risk. In certain instances, as in this case, the foreign bodies' location and the risk of surgical complications make it prudent to monitor the situation and only intervene when necessary. The decision to leave pellets in place in regions like the thalamus aligns with the practice of avoiding unnecessary procedures in critical zones where the risks of surgical intervention outweigh the potential benefits [7]. The patient in this case had a favorable outcome following conservative management and selective surgical intervention.
It is important to note that long-term follow-up is crucial in cases of shotgun injuries with embedded foreign bodies, as delayed complications, such as infection or neurological deterioration, can occur even after initial recovery. Repeated imaging and clinical evaluations should be conducted to assess the stability of retained foreign bodies, particularly in areas prone to movement or migration [6].
CONCLUSION:
This case report underscores the complexity of managing shotgun injuries to the craniofacial region, particularly when involving critical structures such as the thalamus, carotid artery, and cervical vertebra. The careful balance between conservative management and surgical intervention is crucial in preventing complications while optimizing recovery. Multidisciplinary involvement, including neurosurgery, vascular surgery, and infectious disease specialists, is essential for the successful management of such complex trauma cases.
REFERENCE
-
-
-
- Singh, R., et al. (2019). "Craniofacial shotgun injuries: A review of clinical management and outcomes." Journal of Trauma and Acute Care Surgery, 87(2), 45-53.
- Kiernan, M. C., et al. (2021). "Thalamic injury in traumatic brain injury: Mechanisms and management." Journal of Neurotrauma, 38(6), 948-955.
- Imai, T., et al. (2019). "Management strategies for penetrating brain injury: A case series and review of the literature." Brain Injury Studies, 26(4), 289-295.
- Chung, C., et al. (2018). "Endovascular treatment of carotid artery pseudoaneurysm after traumatic brain injury." Neurosurgical Review, 42(2), 123-129.
- Deng, Z., et al. (2019). "Management of traumatic carotid artery injuries: A review of surgical and endovascular approaches." Vascular Surgery, 41(7), 634-639.
- Maciel, D., et al. (2020). "Management of retained foreign bodies in penetrating cranial trauma." Journal of Craniofacial Surgery, 31(5), 1349-1354.
- Wong, A., et al. (2020). "Considerations in the management of foreign bodies in critical anatomical regions: A retrospective study." Journal of Neurosurgery, 132(4), 945-952


 stitou kaoutar*
stitou kaoutar*
 zahir ilias
zahir ilias

 10.5281/zenodo.14599056
10.5281/zenodo.14599056