Abstract
Chronic skin diseases are a diverse group of long-lasting or recurrent conditions that affect the skin, leading to significant physical, emotional, and social challenges for individuals. These conditions are often marked by persistent inflammation, impaired skin barrier function, and immune dysregulation. Some of the most common chronic skin diseases include psoriasis, atopic dermatitis (eczema), acne vulgaris, rosacea, chronic urticarial, and hidradenitis suppurativa. While each disease presents with distinct symptoms and pathophysiology, they share common features, including a tendency to relapse over time, the potential for a significant impact on quality of life, and the need for long-term management.
Keywords
Chronic skin diseases, psoriasis, eczema, acne vulgaris, rosacea, immune dysregulation, management, quality of life, treatment.
Introduction
Chronic skin diseases refer to a range of long-lasting conditions that affect the skin, often causing discomfort, aesthetic concerns, and sometimes severe health implications. These disorders can include conditions like eczema, psoriasis, acne vulgaris, rosacea, and chronic urticaria, among others. Chronic skin diseases are typically characterized by persistent or recurrent inflammation, immune system dysregulation, and skin barrier dysfunction. They may result from a complex interaction of genetic, environmental, and lifestyle factors, with symptoms ranging from redness, itching, and scaling to more severe manifestations such as ulcerations or thickened skin. While chronic skin conditions are not usually life-threatening, they can significantly impact the quality of life, leading to emotional distress and social stigmatization. Treatment strategies often involve topical therapies, systemic medications, and lifestyle modifications to manage symptoms, reduce flare-ups, and improve the skin’s appearance and function. Early diagnosis and personalized treatment are crucial for managing these disorders effectively.
Vitiligo, a depigmenting skin disease, is characterized by the selective loss of melanocytes, which successively ends up in pigment dilution within the affected areas of the skin. The characteristic lesion may be an altogether amelanotic, nonscaly, chalky-white speckle with distinct margins. Tidy recent progress has been created in our understanding of the Pathological process of skin condition, and it’s currently clearly classified as a disease, related To genetic and environmental factors at the side of metabolic, aerophilic stress and cell Detachment abnormalities {vitiligo|skin sickness|disease of the skin|skin disorder|skin Problem|skin condition} mustn’t be pink-slipped as a cosmetic or insignificant disease, as its Effects will be psychologically devastating, usually with a substantial burden on standard of Living. Vitiligo, a depigmenting skin disease, is characterized by the selective loss of Melanocytes that successively ends up in pigment dilution within the affected areas of the Skin. The characteristic lesion may be an altogether amelanotic, nonscaly, chalky-white speckle with distinct margins. Tidy recent progress has been created in our understanding of the Pathological process of skin condition, and it’s currently clearly classified as a disease, related To genetic and environmental factors at the side of metabolic, aerophilic stress and cell Detachment abnormalities {vitiligo skin disease of the skin disorder skin Problem skin condition} mustn’t be pink-slipped as a cosmetic or insignificant disease, as its Effects will be psychologically devastating, usually with a substantial burden on the standard of living.
-
- Segmental skin condition:
It’s additionally referred to as unilateral or localized vitiligo. The white patches solely affect one space of your body. It is additionally common in youngsters from three to Ten years old.

Fig. Segmental Vitiligo.
-
- Non-segmental skin condition: It is additionally referred to as bilateral or generalized skin condition. The symptoms usually seem on each of your body. It’s seen on your body hands, arms, skin, around the body gap like an eye.

Fig. Non Segmental Vitiligo
- Etiology
Chronic skin diseases can arise from a variety of etiological factors, including genetic, environmental, immunological, and infectious causes. Genetic predisposition plays a significant role in many chronic skin conditions, such as psoriasis, atopic dermatitis, and vitiligo. Individuals with a family history of skin diseases are more likely to develop similar conditions, indicating a hereditary component. Environmental factors also contribute to the development and exacerbation of chronic skin diseases. These include prolonged exposure to ultraviolet (UV) radiation, which can trigger or worsen conditions like lupus and actinic keratosis. Environmental allergens, irritants, and pollutants can also provoke allergic reactions or sensitivities, leading to conditions such as eczema and contact dermatitis. Immunological dysfunction is another critical factor in many chronic skin diseases. For example, autoimmune conditions like lupus erythematosus and scleroderma occur when the body’s immune system mistakenly attacks its tissues. In conditions like psoriasis, immune cells are activated inappropriately, leading to inflammation and rapid skin cell turnover. Infectious agents, including bacteria, fungi, and viruses, can also contribute to the persistence of skin conditions. For instance, chronic fungal infections like dermatophytosis can cause long-term skin damage, while viral infections like herpes simplex virus may result in recurrent flare-ups of conditions such as eczema herpeticum. Other contributing factors include hormonal imbalances, stress, and nutritional deficiencies, which can exacerbate conditions like acne and seborrheic dermatitis. In some cases, medications or lifestyle factors such as smoking can worsen chronic skin conditions. Overall, the etiology of chronic skin diseases is multifactorial, with complex interactions between genetic predisposition, environmental triggers, immune system dysfunction, and infections. Effective management often requires addressing these various underlying causes.
- Symptoms and Cause
Chronic skin diseases are characterized by persistent symptoms that can vary depending on the specific condition. Common symptoms include redness, inflammation, itching, dryness, scaling, and thickening of the skin. In some cases, lesions or rashes may develop, and there could be pain or discomfort, especially with conditions like eczema or psoriasis. Chronic skin diseases can also result in changes to skin texture, discoloration, and scarring, leading to potential psychological and emotional effects such as anxiety or depression. The causes of chronic skin diseases are multifactorial. Genetic factors often predispose individuals to conditions like psoriasis, atopic dermatitis, or vitiligo. Environmental triggers, including allergens, irritants, and UV radiation, can exacerbate or initiate flare-ups. Immune system dysfunction is a key cause of autoimmune-related skin disorders like lupus and scleroderma, where the body attacks its tissues. Infections caused by bacteria, fungi, or viruses (e.g., fungal dermatitis or herpes) can lead to chronic conditions. Hormonal changes, stress, poor diet, or smoking can further exacerbate skin problems. Some medications and underlying systemic diseases also contribute to skin conditions, making management complex. Effective treatment requires addressing the underlying cause and symptom relief.
4. HOW FAST DOES THE DISEASE SPREAD?
The rate at which a chronic skin disease spreads or worsens depends on the specific condition and its underlying causes. Unlike acute infections, which can spread rapidly, chronic skin diseases generally progress more slowly and may have periods of flare-ups and remission.
- Psoriasis: This autoimmune condition involves rapid skin cell turnover, leading to the formation of thick, scaly patches. The disease itself doesn’t “spread” in the traditional sense, but new lesions can appear over time, and flare-ups can be triggered by stress, infections, or environmental factors.
- Eczema (Atopic Dermatitis): Eczema is typically characterized by flare-ups that may worsen with exposure to allergens or irritants. While it doesn’t spread from person to person, the severity of symptoms can fluctuate over time, and lesions may spread to other areas of the body if triggers are not managed.
- Vitiligo: This condition causes patches of skin to lose pigment. It often progresses slowly, and the rate at which it spreads varies widely between individuals. In some cases, the loss of pigment may be stable for years, while in others, it may spread rapidly.
- Lupus: Lupus is a systemic autoimmune disorder that can affect the skin along with other organs. Skin involvement tends to develop slowly, with periodic flare-ups that may worsen during periods of stress or illness.
Overall, the progression or spread of chronic skin diseases varies based on the individual, the disease, and environmental factors. Treatment and management play a significant role in controlling and slowing disease progression.
5. New advances in management:
5.1 Medical therapies:
NB-UVB Recent medical advances have included narrow-band ultraviolet-B (NB-UVB) Therapy, targeted ultraviolet-B (UVB), excimer laser therapies, topical treatment with Immunomodulatory in the form of topical calcineurin inhibitors, topical pseudo catalase and Topical vitamin D analogs in combination with UV light.NB-UVB using UV lamps with peak emission around 311nm is now the first-line treatment For generalized vitiligo and vitiligo vulgaris (patchy vitiligo). The effectiveness of NB-UVB In vitiligo was first demonstrated in 1997 by Westerhof and Nieuwboer-Krobotova. Since then, there have been numerous clinical studies that have demonstrated the therapeutic Benefits of NB-UVB in vitiligo patients. The mechanism of action of NB-UVB in vitiligo is based on the induction of local immunosuppression. And stimulation of melanocyte Proliferation in the skin and the outer root sheath of hair follicles. There is a stimulating effect on melanogenesis and on the production of melanocyte-stimulating hormone (MSH). Comparative studies have shown a significantly higher repigmentation rate with NB-UVB Compared to topical therapy with psoralen and ultraviolet A (PUVA). In addition, the Frequency of side effects commonly observed with topical PUVA, such as B. Phototoxicity, was significantly reduced by the use of NB-UVB.
5.2 Laser Therapy :
The excimer laser, which uses xenon-chlorine gas (Xe-Cl) and produces a monochromatic laser Light with a wavelength of 308 nm, is another innovative treatment option for vitiligo. The laser System has been used more and more frequently in recent years. For the targeted treatment of Individual vitiligo lesions. The laser is used alone or in combination with a topical Immunomodulatory or PUVA sol therapy. Treatment with this laser is said to give extremely good and early results in both localized and segmental vitiligo. Repigmentation was better on the face and trunk than on the extremities. Topical therapies, particularly topical tacrolimus, have been used in combination with the excimer laser. This combination is said to be more effective than the excimer laser alone. In a randomized right-left comparative study with 14 Patients, excimer light monotherapy was compared with a combination of excimer laser and Topical tacrolimus.
5.3 Topical Vitamin D analogs:
Vitamin D analogs, specifically calcipotriol, have been used topically in the treatment of Vitiligo either alone or in combination with topical steroids. The reason for using these funds Is that vitamin D3 affects the growth and differentiation of both melanocytes and Keratinocytes. This was further demonstrated by the detection of receptors for 1-alpha-Dihydroxyvitamin D3 on melanocytes. These receptors are thought to play a role in stimulating melanogenesis. Vitamin D analogs have given different results in the treatment of vitiligo in different studies. These agents have also been used in combination with Ultraviolet light (including NB-UVB) and topical steroids with variable results.
5.4 Melanocyte culture transplantation :
This is a relatively more advanced transplantation procedure, in which a split-thickness skin graft is Harvested from a donor area and incubated in a suitable culture medium to grow the melanocytes or a Combination of keratinocytes and melanocytes in vitro. The cultured cells are then applied to the injured skin by laser dermabrasion or even mechanical abrasion. The method is more difficult to perform as it requires advanced laboratory facilities for culturing melanocytes. However, the results with this procedure are excellent and a relatively large area of affected skin can be treated with a single donor graft.

Fig. Depigmentation of the fingers and dorsum of the hands, classical, early manifestations of vitiligo.
6. Current treatment:
Current treatments for chronic skin diseases focus on controlling symptoms, reducing inflammation, and preventing flare-ups, with approaches tailored to the specific condition. Topical treatments are commonly used for many chronic skin conditions. These include corticosteroids, which help reduce inflammation and itching, and calcineurin inhibitors for conditions like eczema. Topical retinoids may be used for psoriasis and acne, promoting cell turnover and reducing scaling. Systemic treatments are often necessary for more severe or widespread chronic skin conditions. For psoriasis, biologic drugs (e.g., adalimumab, ustekinumab) have become the standard for moderate to severe cases, targeting specific immune system components to reduce inflammation and slow skin cell turnover. Immunosuppressants such as methotrexate and cyclosporine may be prescribed for autoimmune conditions like psoriasis and eczema, although their use is typically limited by side effects. Oral antibiotics or antifungal treatments are used when infections, such as bacterial or fungal dermatitis, contribute to skin disease. For eczema, moisturizers play a critical role in managing dry, inflamed skin. Phototherapy (UV light treatment) is another option for conditions like psoriasis and atopic dermatitis, where controlled exposure to UV light helps reduce inflammation and slow down excessive skin cell production. Additionally, addressing environmental triggers is crucial in managing chronic skin diseases. Allergen avoidance, stress management, and lifestyle changes, including a healthy diet and proper skin care routines, can significantly improve outcomes. In the case of vitiligo, treatments may include topical steroids, phototherapy, or skin grafting in some cases. Research into gene therapy and JAK inhibitors offers hope for future treatments. Overall, effective management often involves a combination of therapies personalized to the patient’s specific needs and disease severity.
7. Risk Factors for Vitiligo:
These factors are known to increase the risk for vitiligo:
? Family history and genes about 20 percent of people with vitiligo have at least one Close relative affected by the skin condition, and researchers have found that people with a certain genetic profile are more prone to developing vitiligo. Variations in More Than 30 genes associated with vitiligo have been identified, including two named NLRP1 and PTPN22, according to MedlinePlus. These and other genes now associated with vitiligo are known to be involved in the regulation of the immune system and Inflammation.
? Environmental Triggers Vitiligo appears to be the result of both a pre-existing genetic Makeup and something in the environment that triggers an autoimmune response that Destroys melanocytes. Possible triggers include sunburn, exposure to certain Chemicals, and trauma or injury to the skin, according to the F1000 Research article.
8 Pathogenesis:
8.1 Genetics:
The observation that vitiligo was more common in the immediate relatives of vitiligo Sufferers provided early evidence of its heritability. While vitiligo affects approximately 1% of the general population, the risk of a sibling developing the disease is 6% and identical twins 23%. In addition, vitiligo patients and their loved ones are at increased risk of developing other autoimmune diseases, including autoimmune Thyroiditis, type 1 diabetes, pernicious anemia, and Addison’s disease, suggesting that Vitiligo is an autoimmune disease as well. These early observations were subsequently Confirmed by genome-wide association studies (GWA) that identified numerous common Genetic variants in vitiligo patients that encode components of the innate (NLRP1, IFIH1, CASP7, C1QTNF6, TRIF) and adaptive immune systems &# 40; FOXP3, BACH2, CD80, CCR6, PTPN22, IL2R, alpha GZMB, HLA Class I and II) see also Spritz R, Andersen G: Genetics of Vitiligo; in this issue.
8.2 Oxidative Stress:
Several evidence suggest that melanocytes from vitiligo patients have intrinsic defects That reduce their ability to cope with cellular stress reviewed in reactive oxygen Species (ROS). While healthy melanocytes can mitigate these stressors, Melanocytes from vitiligo patients appear to be more vulnerable—the structure of the Melanosome is all characteristic of high cellular stress. High levels of epidermal H2O2 Levels and reduced levels of catalase, a key enzyme that protects cells from oxidative damage, have been observed in the skin of patients with vitiligo.
8.3 Innate immunity:
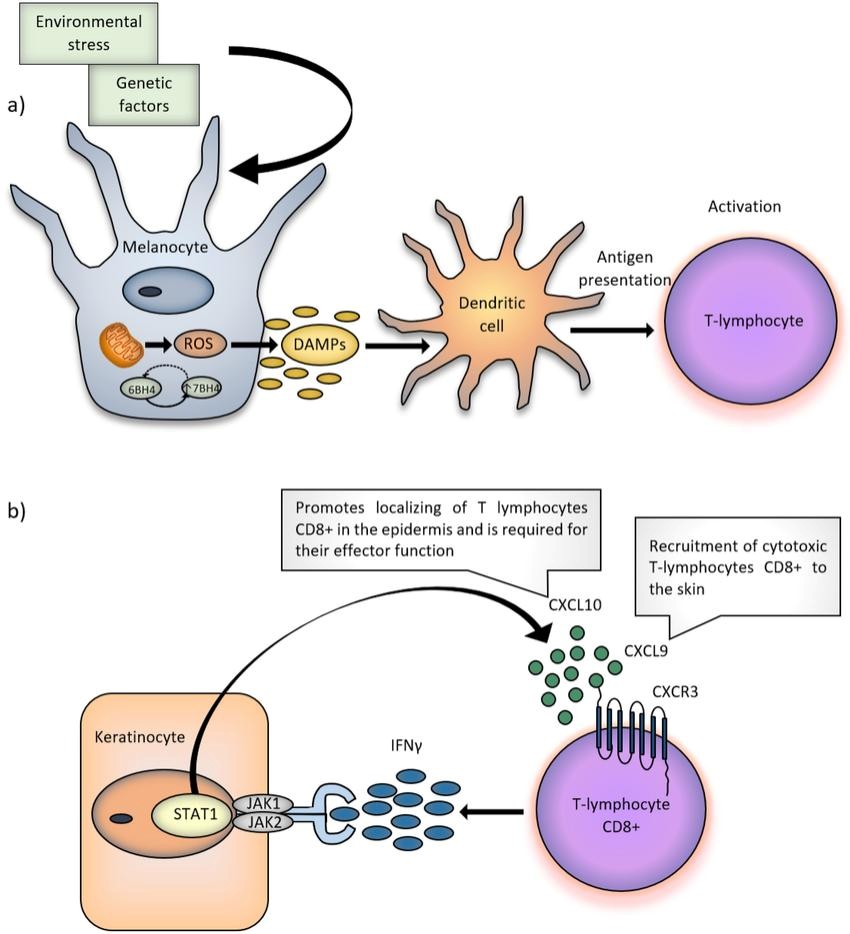
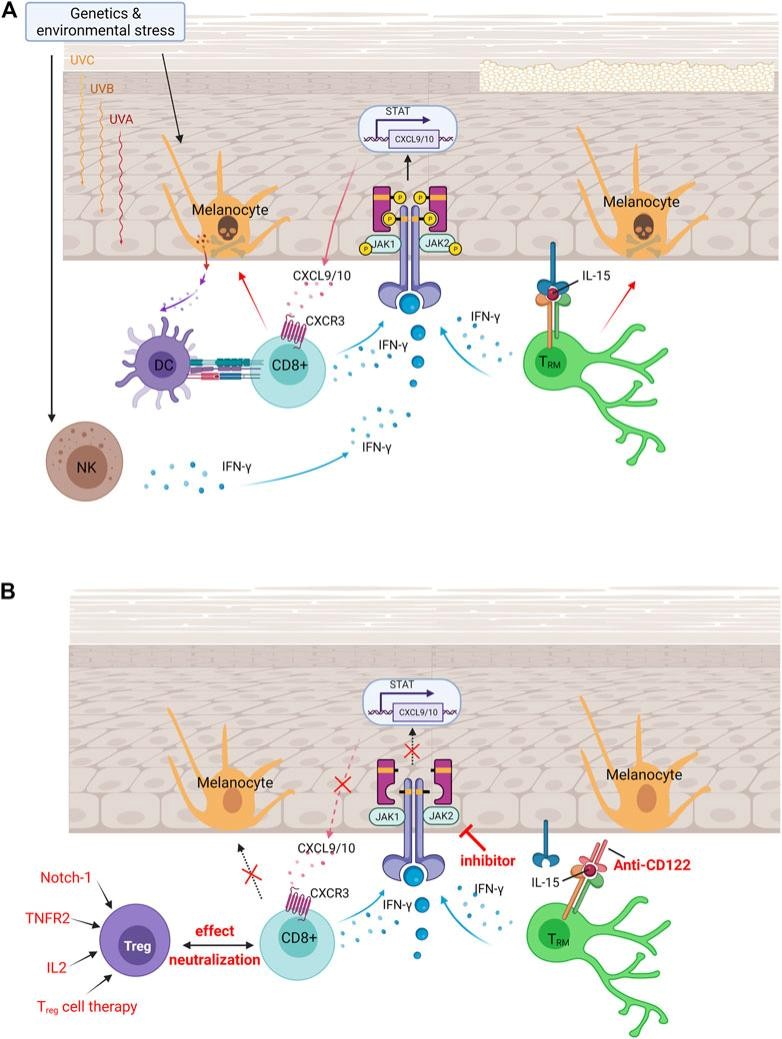
As mentioned above, studies of GWA in patients with vitiligo have implicated multiple Susceptibility sites linked to genes that control innate immunity. This likely causes Dysregulated innate activation in response to stress of melanocytes, as shown by the Recruitment of innate populations such as natural killer (NK) cells and the production and Release of high levels of pro-inflammatory proteins and cytokines, including shock proteins (HSP), IL -1?, IL6 and IL-8, and are reviewed in FIG. unique in that it can be secreted to Specific companion peptides of the original host cells. Recently, HSP70i was shown to be important for the pathogenesis of vitiligo in a mouse model through the induction of Inflammatory dendritic cells (DCs), which can either be cytotoxic or carry melanocyte-Specific antigens and present T cells in lymphoid tissues. It has been suggested that this is an Important crosstalk step between innate and adaptive immunity leading to T cell-mediated Autoimmune destruction of melanocytes. There are three goals to consider during the treatment of vitiligo: 1) Reducing melanocyte Stress and 2) suppressing autoimmune targeting of melanocytes. 3) promoting melanocyte Regeneration.
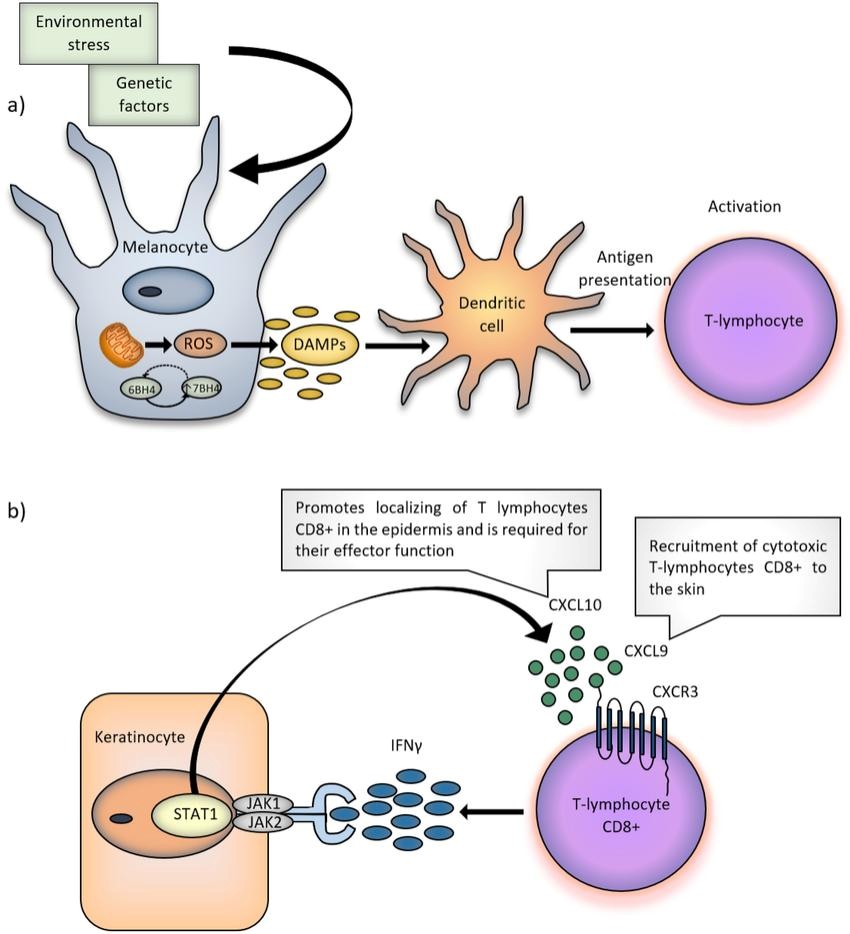
Figure 4: Vitiligo pathogenesis begins with altered melanocytes that exhibit elevated cellular stress Responses.
8.4 Reducing melanocyte stress:
The apparent reduction in catalase enzyme in the epidermis of vitiligo patients, as well as increased levels of ROS in damaged skin, led to the hypothesis that treating patients with Antioxidants or otherwise controlling ROS could be an effective treatment strategy. Pseudo catalase describes a treatment cream composed of any number of metal ions capable of Converting H2O2, a common ROS, into water and oxygen. Early studies of pseudo catalase in Combination with phototherapy in vitiligo patients seemed promising, however, they were not controlled or blinded and subsequent studies have not reproduced positive results. Results. It is not clear whether this strategy could be optimized or improved for the development of Future therapies. Natural health products, vitamins, and oral or topical supplements have been suggested as possible therapies for their antioxidant and anti-inflammatory properties and are discussed in this issue, Grimes PE, Nashawati R: The role of diet and supplements in vitiligo Management. The herbal supplement Gingko Biloba has been tested in 2 small studies and Reported to promote some improvement. Polypodium leucotomos plant extract was reported to improve response to nbUVB in a small group of vitiligo patients compared to placebo. One Group tested nbUVB with or without supplementation with an “antioxidant pool” containing ?-lipoic acid, vitamin C, vitamin E, and polyunsaturated fatty acids. They reported greater Efficacy in patients who received a combination of nbUVB plus antioxidants. Larger Controlled studies are needed to determine if antioxidant supplementation is a beneficial Strategy to complement patient management.
9. Regulating autoimmunity
Over the past decade, significant advances have been made in the development of Immunomodulatory to treat inflammatory skin diseases, including more targeted Treatments. Recent advances in our understanding of vitiligo immune pathogenesis have Helped us identify new immune targets to develop and test new vitiligo treatments.
9.1 HSP70i:
One group reported a role for the heat shock protein HSP70i in the pathogenesis of vitiligo, suggesting that it is released from stressed melanocytes and triggers congenital inflammation In the skin. They then discovered that when expressed in the skin of a mouse model, the Protein mutation made it less immunogenic and even appeared to induce tolerance, thereby preventing the onset of the disease. They suggested testing this as a new treatment for vitiligo in The future, although transferring DNA from a mutated protein to the skin of patients could take time to develop and prove safe.
9.2 IFN-?/CXCL10:
We previously reported that the IFN-?/CXCL10 axis is a critical signaling pathway required for both progression and maintenance of vitiligo, and we hypothesized that targeting this Pathway could be an effective treatment strategy. A variety of antibodies and small molecule Inhibitors have been developed to target components of this pathway (including IFN-?, CXCL10, and theCXCL10 CXCR3 receptor) and have been found safe in early clinical trials For the treatment of other autoimmune diseases such as psoriasis, rheumatoid arthritis and Crohn’s disease. Most of these studies did not meet their efficacy endpoint, probably because IFN-? is not an important cytokine that leads to these diseases. However, recent results in Patients and a mouse model suggest that vitiligo is an optimal disease drug.
9.3 JAK-STAT signaling:
JAK-STAT signaling is essential for the transmission of extracellular signals from many Cytokines, including IFN-?, to the cell nucleus. After cytokine receptor ligation, Janus kinases (JAKs) phosphorylate signal transducer and transcription activator (STAT) proteins, which become activated and induce transcription of target genes. There are four members of the JAK family including JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2). Among these, JAK1 and JAK2 are directly involved in IFN-? signaling, which activates STAT1 and thus reduces transcription of IFN-?-induced genes, including CXCL10.
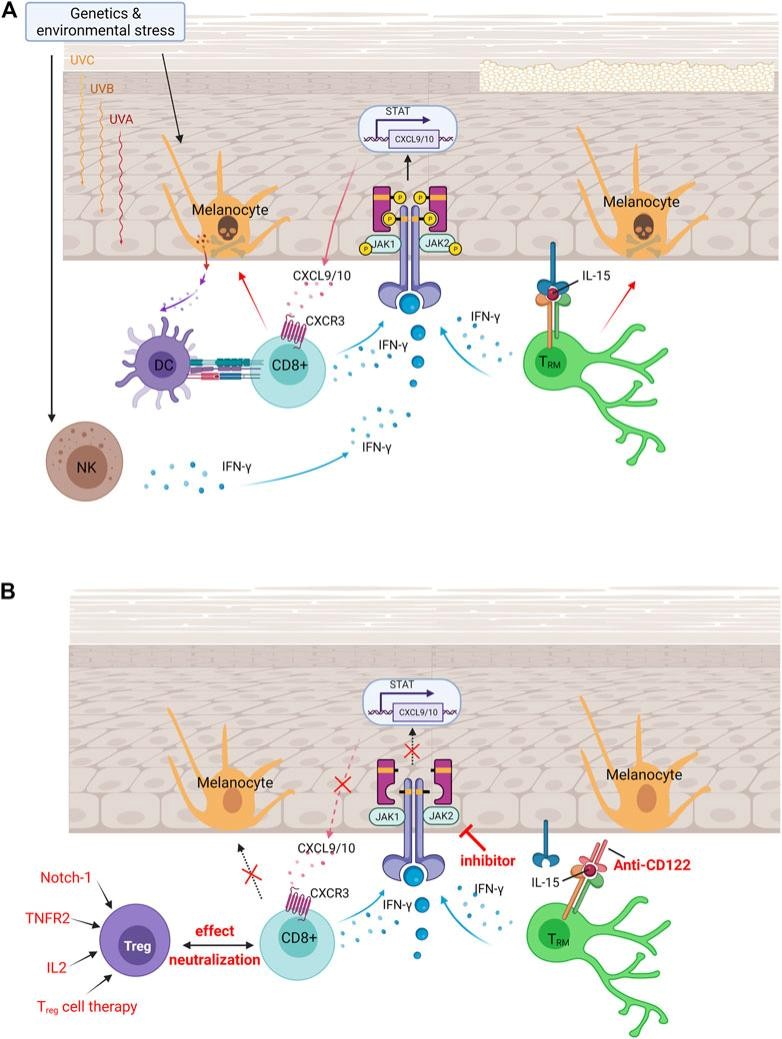
Figure: Autoimmunity in vitiligo is driven by the IFN -y-CXCL 10 Cytokine signaling pathway.
OBJECTIVE
The objective of chronic skin disease management is to address both the medical and psychosocial aspects of the condition, aiming for:
1. Symptom Relief: Minimize symptoms like itching, pain, redness, scaling, or dryness.
2. Disease Control: Slow disease progression or prevent flare-ups.
3. Improved Skin Integrity: Heal and maintain healthy skin, reducing complications such as infections or scarring.
4. Enhance Quality of Life: Address physical discomfort, social stigma, and emotional distress caused by the condition.
5. Long-term Management: Develop sustainable treatment strategies, such as medications, lifestyle changes, or therapies.
6. Patient Education: Empower patients to manage their condition, adhere to treatments, and recognize triggers.
7. Prevention of Complications: Avoid secondary infections, systemic involvement, or permanent skin damage.
CONCLUSION
Chronic skin diseases, such as eczema, psoriasis, and rosacea, are long-lasting conditions that significantly impact physical and emotional well-being. Although these conditions often cannot be cured, they can be managed through proper treatment, lifestyle adjustments, and consistent care. Early diagnosis and tailored therapies, including topical medications, systemic treatments, and lifestyle modifications, are crucial in minimizing symptoms and improving quality of life. Additionally, addressing the psychological impact of chronic skin conditions through support groups or counseling is essential. Advances in dermatology continue to offer hope for better management options, emphasizing the importance of ongoing research and patient-centered care.
Acknowledgment:
We are thankful to Arihant College of Pharmacy, Ahilyanagar. For providing us with the platform and infrastructure for preparing this article also thanks to our Principal Dr. Yogesh Bafana sir, and Assistant Professor Ms. Sneha S. Kanase & Mr. Swapnil Kale for their support and expert opinion during the writing process.
REFERENCE
- Christina Bergquist ,Ezzedinek . karger dermatology. Review of vitiligo 2020 , Vol.236 No.6
- Boisseau-Garsaud AM, Garsaud P, Calès-Quist D, Hélénon R, Quénéhervé C, Claire RC. Epidemiology of vitiligo in the French West Indies (Isle of Martinique). Int J Dermatol. 2000 Jan;39(1):18–20.
- Hauz khas. International journal of pharmaceutical research and medicinal Plants. July- August 2018,vol.1(4) pg no.72-75.
- Sk Sarkar ,KG sen ,MK mostofa,Review on vitiligo manangement An Update.july2017(12)(1), pg no. 34-39
- J. Dermatol . Indian journal of dermatology . march-april 2011 56(2) pg no. 180-189.
- Picardo M, Dell’Anna ML, Ezzedine K, Hamzavi I, Harris JE, Parsad D, et al.Vitiligo. Nat Rev Dis Primers. 2015 Jun;1(1):15011.
- Ezzedine K, Grimes PE, Meurant JM, Seneschal J, Léauté-Labrèze C, Ballanger F, et al. Living with vitiligo: results from a national survey indicate Differences between skin phototypes. Br J Dermatol. 2015 Aug;173(2):607–9.
- Mehdi rashighi MD, John Harris MB , HHS public Access .author manuscript Bypeer review and accepted for publication.nov.2016.
- Mini review article frontiers immunology in vitiligo updated on therapeutic Target 31 August 2022
- Nordlund JJ, Ortonne JP. Vitiligo vulgaris. In: Nordlund JJ, Hearing VJ, King RA, Oetting W, Ortonne JP, editors. The pigmentary system: Physiology and Pathophysiology. Oxford: Blackwell Scientific, Inc; 2006. Pp. 591–8. [Google Scholar].
- Hann SK, Nordlund JJ, editors. 1st ed. Oxford, London: Blackwell Science Ltd;2000. Vitiligo: A Monograph on the Basic and Clinical Science; pp. 1–386. [Google Scholar].
- Frisoli ML, Essien K, Harris JE. Vitiligo: Mechanisms of Pathogenesis and Treatment. Annu Rev Immunol (2020) 38. Doi: 10.1146/annurev-immunol- 100919-023531.


 Abhishek Bhosale*
Abhishek Bhosale*



 10.5281/zenodo.14250785
10.5281/zenodo.14250785