Abstract
Emerging therapies for oral health represent a significant advancement in the prevention, treatment, and management of oral diseases. Traditional dental practices are being complemented by novel approaches that incorporate biotechnology, regenerative medicine, and biomaterials. These therapies aim to address challenges such as tooth decay, gum disease, oral cancer, and tissue regeneration. Innovations such as stem cell-based treatments, antimicrobial peptides, salivary diagnostics, and gene therapy offer promising alternatives to conventional treatments. Additionally, advancements in bioactive materials, including demineralizing agents and advanced dental restorations, are enhancing the effectiveness of restorative care. This abstract reviews the latest developments in oral health therapies, highlighting their potential to improve patient outcomes, reduce treatment times, and provide more sustainable solutions for oral health management. As research continues to progress, these emerging therapies hold the promise of transforming the future of oral healthcare.
Keywords
Emerging therapies, oral health, biotechnology, regenerative medicine, biomaterials, stem cell treatments, antimicrobial peptides, salivary diagnostics, gene therapy, tooth decay, gum disease, oral cancer, tissue regeneration, bioactive materials, dental restorations, oral healthcare advancements.
Introduction
Oral health refers to the overall health of your mouth, including your teeth, gums, tongue, lips, and the tissues inside your mouth. Good oral health is essential for maintaining a healthy body.
1) Prevents tooth decay: Regular brushing, flossing, and dental check-ups can help prevent tooth decay, which is caused by bacteria that build up on your teeth and produce acids that erode the enamel.
2) Prevents gum disease:
- Gum disease, or periodontal disease, is a serious infection of the gums and bones that support your teeth.
- It can lead to tooth loss, bad breath, and other health problems.
- Brushing and flossing regularly can help prevent gum disease.
3) Boosts self-confidence:
- A healthy smile can boost your self-confidence and make you feel more attractive.
- Poor oral health, such as bad breath or discolored teeth, can affect your self-esteem and social interactions.
4) Reduces the risk of other health problems:
- Poor oral health has been linked to several health problems, including heart disease, diabetes, and stroke.
- Bacteria that cause gum disease can enter the bloodstream and contribute to inflammation.
5) Improves nutrition:
Healthy teeth and gums allow you to chew and digest food properly, which can improve your nutrition and overall health. Maintaining good oral health requires regular brushing, flossing, and dental check-ups.
You should brush your teeth at least twice a day with fluoride toothpaste, floss daily, and visit your dentist regularly for cleanings and check-ups.
*Eating a healthy diet, avoiding sugary and acidic foods, and avoiding tobacco and excessive alcohol can also help maintain good oral health
EMERGING THERAPIES:
Emerging therapies refer to new and innovative treatments that are currently being developed or investigated in clinical trials for various medical conditions. These therapies often use advanced technologies or approaches that are different from those currently used in standard medical practice. The scope of emerging therapies is broad and encompasses various medical fields, including cancer, neurology, cardiovascular disease, infectious diseases, and many others.
Some examples of emerging therapies include:-
- Gene Therapy

2) Cell Therapy
3) Immunotherapy
4) Nanomedicine
5) CRISPR -Cas9
Transitioning from the concept of clinical application to actual implementation is crucial for several reasons:
- Patient Benefits:-
The primary goal of any clinical application is to improve patient care. By transitioning from concept to application, healthcare providers can directly use these tools to diagnose, treat, or manage patient conditions more effectively, leading to improved patient outcomes.
2) Efficiency and Productivity:
Clinical applications can automate routine tasks, reducing the workload of healthcare professionals. This can lead to increased efficiency and productivity, allowing healthcare providers to focus on more complex tasks and spend more time with patients.
3) Quality and Safety:-
Well-designed clinical applications can help improve the quality and safety of healthcare. For example, electronic health records can reduce errors associated with paper records, while telemedicine can improve access to care for patients in remote areas.
4) Cost Savings:-
By automating processes and improving efficiency, clinical applications can lead to cost savings. For example, reducing the need for hospital admissions or improving medication adherence can lead to significant cost savings.
5) Research and Innovation:-
Transitioning clinical applications into practice can also stimulate research and innovation. By seeing how these applications are used in real-world settings, developers can identify areas for improvement and develop new applications to meet emerging healthcare needs.
6) Compliance with Regulations:-
Many countries have regulations requiring the use of certain clinical applications, such as electronic health records. Transitioning to these applications can help healthcare providers comply with these regulations and avoid potential penalties.
7) Patient Satisfaction:-
By providing more convenient, personalized, and efficient care, clinical applications can improve patient satisfaction. This can lead to better patient engagement and adherence to treatment plans.
In an ever-evolving understanding of health, the concept of oral health (OH) has been redefined to extend beyond the condition of the mouth and teeth. :
The World Health Organization (WHO) characterizes OH as pivotal, encompassing not only physical aspects but also psychosocial dimensions that influence essential functions such as eating, breathing, and communication.
This perspective underscores the interplay between OH and broader well-being, accentuating the need for a comprehensive public health approach that addresses the intricate web of determinants shaping OH outcomes.
Central to this is the recognition of the far-reaching impact of OH on individuals’ quality of life and overall health OH has been shown to be linked to various diseases and conditions, many of which are preventable. The WHO’s global OH report (2022) emphasized the significance of conditions like dental caries, severe periodontal diseases, and oral cancer, which reflects the complex landscape of OH challenges, evidence highlights the bi-directional relationships between oral diseases and non-communicable diseases (NCDs), underscoring the common risk factors and the potential for mutual exacerbation The burden of oral diseases surpasses that of major NCDs, signifying the urgent need for targeted interventions It is evident that OH inequalities persist; vulnerable populations, including those living in poverty, children, the elderly, and remote communities, bear a disproportionate share of this burden.
Overview of novel research and emerging ideas:-
One innovative concept in oral health therapies is the use of nanotechnology. Nanotechnology involves the manipulation of materials at the nanoscale, which is about 1 to 100 nanometres in size. In oral health, nanotechnology can be used for various applications such as:-
1) Dental Fillings
2) Antimicrobial coating
3) Tooth Decay Prevention
4) Dental Sensors
Example of a ground-breaking concept in oral health:-
One ground-breaking concept in oral health research is the use of stem cells for regenerative dentistry. Stem cells have the potential to differentiate into various cell types, including dental pulp cells, periodontal ligament cells, and oral epithelial cells. This property makes them an attractive option for regenerating damaged or lost tissues in the oral cavity.
Researchers are investigating the use of stem cells for various dental applications, such as:-
1) Regenerating damaged dental pulp:
2) Tissue engineering:
3) Repairing periodontal ligament:
4) Treating oral mucosal diseases:
Current Trends:-
1. Precision Medicine:-
- Treatments tailored to individual genetic profiles and biomarkers.
- Increased focus on genomics and personalized treatment plans, especially in oncology.
2. Gene Therapy:-
- -Techniques like CRISPR and viral vectors are being used to correct genetic defects.
- -Approved therapies for conditions like spinal muscular atrophy and certain types of inherited blindness.
3. Immunotherapy:-
- Significant advances in cancer treatment using checkpoint inhibitors, CAR-T cell therapy, and monoclonal antibodies.
- Expansion into autoimmune diseases and infectious diseases.
4. Regenerative Medicine:-
- Use of stem cells and tissue engineering to repair or replace damaged tissues and organs.
- Ongoing research into organoids and 3D bioprinting.
5. Digital Health and Telemedicine:-
- Increased use of remote monitoring, telehealth services, and mobile health applications.
- Integration of AI and machine learning for personalized treatment and predictive analytics.
7. RNA-Based Therapies:-
- MRNA vaccines have become prominent, especially for COVID-19.
- Ongoing research into RNA interference and antisense oligonucleotides for other diseases
Future Direction:-
- Combination Therapies:-
The future may see a rise in the use of combination therapies that integrate multiple modalities, such as immunotherapy with traditional chemotherapy or targeted therapies.
- Regenerative Medicine:-
Advances in 3D bioprinting and tissue engineering may lead to the development of lab-grown organs and tissues, addressing transplant shortages and improving repair mechanisms.
- Vaccine development:-
The rapid development of mRNA vaccines for COVID-19 could lead to new platforms for vaccines against other infectious diseases and cancers.
Role Of Phytochemicals In Maintaining Oral Health:-
Phytochemicals are naturally occurring compounds found in plants that exhibit various biological activities with potential health benefits. Several phytochemicals have been shown to play a role in maintaining oral health and preventing oral diseases. Here are some examples:-
1)POLYPHENOLS:- Polyphenols, such as tannins, flavonoids, and catechins, are abundant in green tea, red wine, fruits, and vegetables. They have been demonstrated to inhibit the growth of oral pathogens, reduce plaque formation, and prevent dental caries.
2) ESSENTIAL OIL: - Essential oils derived from plants, including clove, eucalyptus, and peppermint, have antimicrobial and anti-inflammatory properties and may help maintain oral health by reducing bacterial load and promoting gingival health.
3) CURCUMIN: - Curcumin, the active ingredient in turmeric, has anti-inflammatory, antioxidant, and antimicrobial properties. It has been shown to reduce inflammation and oxidative stress in periodontal tissue, as well as inhibit the growth of oral pathogens.
Phytochemicals, naturally occurring compounds in plants, have been studied for their potential therapeutic effects on oral health. Here are some specific phytochemicals and their roles:-
1. Flavonoids:-
- Source: - Found in fruits, vegetables, tea, and red wine.
- Effect: - Exhibits antibacterial properties that can inhibit the growth of oral pathogens like Streptococcus mutants, reducing plaque formation and the risk of cavities.
2. Polyphenols:-
- Source: - Present in green tea, berries, and apples.
- Effect: - Antioxidant and anti-inflammatory properties that can help reduce gingivitis and periodontal
Alicen:-
- Source: - Derived from garlic (Allium sativum).
- Effect: - Antimicrobial properties that can combat oral pathogens and help in the prevention of periodontal diseases.
4. Curcumin:-
- Source: - Found in turmeric (Curcuma longa).
- Effect: - Anti-inflammatory and antibacterial effects that may help in managing oral diseases like gingivitis and periodontitis.
5. Resveratrol:-
- Source: - Present in red grapes, berries, and peanuts.
- Effect: - Antioxidant properties that may support periodontal health by reducing inflammation and modulating immune responses.
6. Saponins:-
- Source: - Found in legumes and some herbs.
- Effect: - Antimicrobial activity against various oral bacteria, potentially aiding in plaque control and oral hygiene.
7. Tannins:-
- Source: - Present in tea, coffee, and some fruits.
- Effect: - Antimicrobial properties that can help reduce oral pathogens and enhance oral health.
8. Essential Oils (e.g., Tea Tree Oil):-
- Source: - Extracted from the leaves of the tea tree (Melaleuca alternifolia).
- Effect: - Antimicrobial and anti-inflammatory properties that can help in treating gingivitis and other oral infections.
Therapeutic Applications:-
Mouthwashes and Rinses: Many of these phytochemicals are used in herbal mouthwashes to enhance oral health and reduce bacterial load.
Dental Products: Some toothpaste and dental gels incorporate these phytochemicals for their antibacterial and anti-inflammatory effects. Dietary Approaches: Consuming foods rich in these phytochemicals may provide preventive benefits for oral health. Moringa oleifera, commonly known as the drumstick tree or miracle tree, is recognized for its nutritional and medicinal properties. Emerging research highlights its potential applications in oral health, particularly for periodontal disease. Here’s an overview of Maringa’s benefits and emerging therapies related to periodontal health:
Applications in Periodontal Disease:-

1. Antimicrobial Properties
2. Anti-inflammatory Effects
3. Antioxidant Activity
4. Tissue Regeneration
5. Plaque Control
Nanotechnology in oral health:-
Nanotechnology holds promise for advanced diagnostics, targeted drug delivery, and biosensors. In the long term, medical Nano robots will allow instant pathogen diagnosis and extermination, individual cell surgery in vivo, and improvement of natural physiological function. Current research is focusing On Science is undergoing yet another change, in helping mankind enter a new era, the era of nanotechnology.
- "Nano" is derived from the Greek word for 'dwarf' is a prefix that literally refers to
- 1 billionth of a physical size.
- One nanometre (nm) is a unit of length that equals 1 billionth of a meter.
- Given that a single hair strand has a thickness of 100,000 nm, it becomes easier to visualize what is meant by “Nano” and to understand its significance.
- The size of atoms is approximately 0.1 nm.
- Considering that the size of a usable nanostructure is 1 to 100 nm, it is clearly seen that the area of nanotechnology works at the level of atoms and molecules.
- Nanotechnology is the science of manipulating matter measured in the billionths of meters or nanometre, roughly the size of 2 or 3 atoms
- Similar to nanomedicine, the development of Nano dentistry will allow nearly perfect oral health by the use of nanomaterials and biotechnologies, including tissue engineering and Nano robots
- Nanomaterials have garnered significant interest in the field of nanotechnology, and their application in oral health is proving to be quite promising.
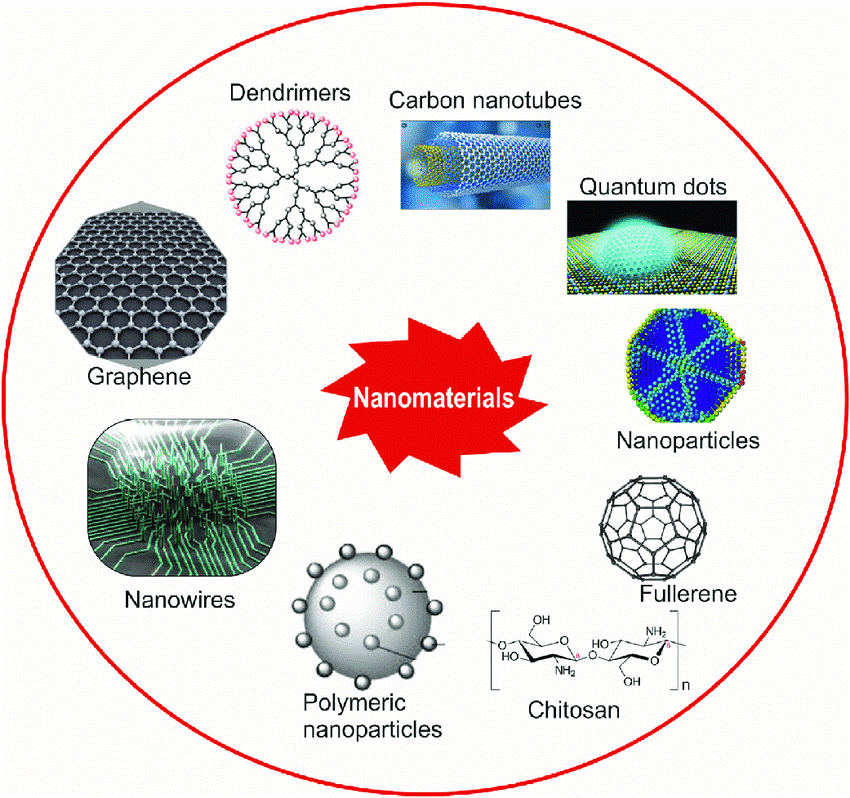
Types of Nanomaterials:
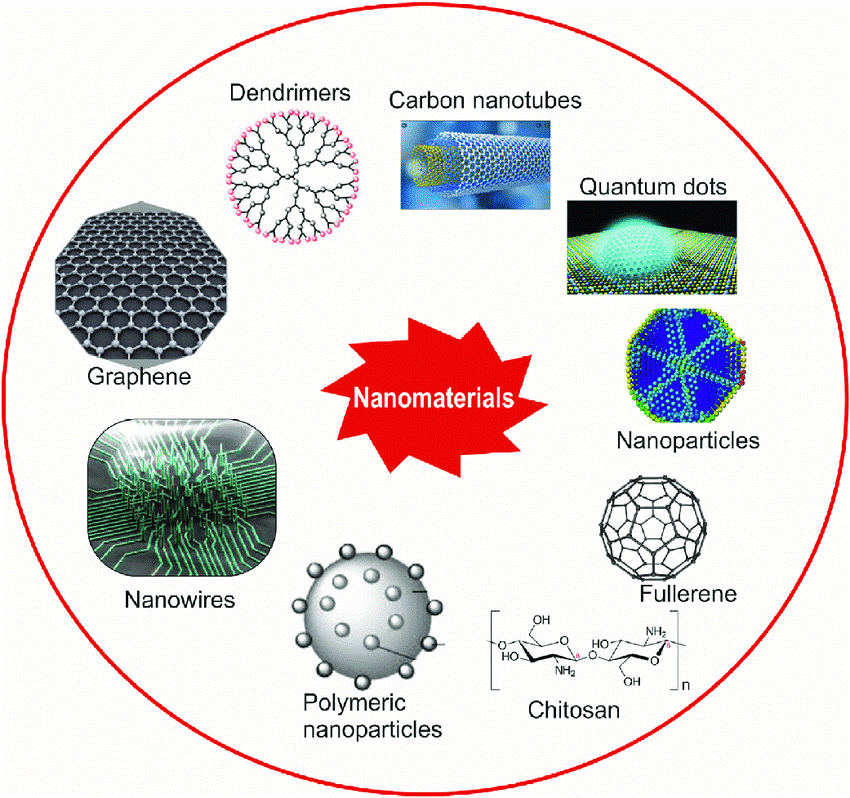
1) Nanoparticles:-
- Tiny particles ranging from 1 to 100 nanometres in size.
- Common examples include silica, titanium dioxide, and silver nanoparticles.
2) Nanotubes:-
Cylindrical nanostructures, such as carbon nanotubes, which have high strength and electrical conductivity.
3) Nanowires:-
Wire-like structures at the nanoscale, often used in sensors and diagnostic tools.
4) Nano sheets:-
Thin, flat nanomaterials, such as graphene oxide, which can be used in various applications due to their high surface area and unique properties.
Applications in Oral Health:-
1) Toothpaste and Oral Care Products:-
a) Fluoride Delivery: - Nanoparticles can enhance fluoride’s effectiveness in demineralizing tooth enamel and preventing cavities.
b) Whitening Agents: - Nanomaterials can improve the whitening process by more effectively breaking down stains on teeth.
2) Dental Restorative Materials:-
a) Composite Resin: - Nanocomposites offer improved mechanical properties and aesthetic qualities for fillings and bonding materials.
b) Dental Cements: - Nanomaterials improve the strength and durability of dental cements used in crowns and bridges.
3) Antimicrobial Treatments:-
A) Silver Nanoparticles: - Known for their antimicrobial properties, these nanoparticles can be incorporated into dental products to reduce bacterial growth and prevent infections.
4) Diagnostics:-
a) Nano-based Sensors: - These can be used for early detection of oral diseases by identifying specific biomarkers or changes in oral health conditions with high sensitivity.
5) Drug Delivery Systems:-
a) Targeted Delivery: - Nano carriers can deliver medications directly to affected areas, such as drugs for treating periodontal disease or managing oral pain.
6) Protective Coatings:-
a) Enamel Protection: Nano coatings can be applied to teeth to provide additional protection against erosion and decay.
7) Regenerative Medicine:
a) Tissue Engineering: - Nanomaterials are used in scaffolds for regenerating dental tissues, such as bone and dentin, to support dental implants and repair damaged tissues.
Challenges:-
1) Safety and Biocompatibility
2) Regulatory Standards:
3) Cost:
4) Long-Term Effects:
Benefits and challenges using nanotechnology in oral health:-
1) Advanced Restorative Materials: - Nanotechnology enables the development of dental materials that are stronger, more durable, and better at mimicking natural tooth structure. This includes improved dental composites and bonding agents.
2) Improved Diagnostics: - Nano-based sensors can detect early signs of oral diseases or conditions with high precision.
Biomaterials and tissue engineering:-
This programme will help you to develop advanced knowledge of biomaterials, bioengineering, tissue engineering, medical engineering and related management topics. Delivered by experts from across UCL and eminent visiting lecturers from industry and medical charities, this interdisciplinary programme attracts physical sciences, engineering and life sciences graduates, including those with qualifications in medicine.
Biomaterials Used In Oral Health Play A Crucial Role In Various Dental Procedures And Treatments.
1) Dental Implants:-
Typically made from titanium or titanium alloys, these biomaterials are used to replace missing teeth. They integrate with the jawbone through Osseo integration.
2) Dental Restorations:-
Materials such as dental crowns, bridges, and inlays can be made from ceramics, composites, or metal alloys. Ceramics like porcelain and zirconia are popular due to their aesthetic qualities and biocompatibility.
3) Composite Resins:-
Used in tooth-coloured fillings, these materials are a blend of resins and inorganic fillers. They are ideal for restoring decayed or damaged teeth while matching the natural tooth colour.
4) Dental Cements:-
Materials like glass ionomer, resin ionomer, and zinc oxide-eugenol are used for luting crowns, bridges, and orthodontic appliances, as well as for temporary restorations.
5) Bone Grafting Materials:-
These include autografts (bone taken from the patient's body), allografts (bone from a donor), xenografts (bone from another species), and synthetic materials. They help in regenerating bone tissue for dental implant placement or repair.
6) Guided tissue regeneration material:-
These materials, often made from biodegradable membranes, are used to promote the growth of new bone and tissue in areas affected by periodontal disease or dental implant surgery.
7) Orthodontic Materials:-Includes brackets, wires, and bands, which are often made from stainless steel, nickel-titanium to correct teeth alignment
8) Sealants and Adhesives:
Used to prevent decay and secure restorations, these materials are typically resin-based and designed to bond strongly with tooth enamel and dentin.
Engineering is defined “as an interdisciplinary field that applies the principles of engineering and the life sciences toward the development of biological substitutes that restore, maintain or improve tissue function.”
Tissue engineering is an attractive alternative to the current surgical options discussed previously and relies on stem cell research. Stem cells are capable of self-renewal and differentiation to a more specialized cell type. They can be classified into three different groups based on this differentiation potential. Totipotent stem cells are able to form an entire embryo, including the extraembryonic tissues. Pluripotent stem cells can differentiate into any of the three germ cell layers (endoderm, mesoderm, and ectoderm). A special type of pluripotent stem cell is “induced” pluripotent stem cells (iPSC) that can be generated directly from adult cells. Omnipotent or progenitor stem cells are limited to one defined cell type. Possible applications of tissue engineering in oral and maxillofacial surgery include hard tissue regeneration for dental rehabilitation, soft tissue engineering, nerve regeneration and the reconstruction of major defects, with the possibility of eventual organoid fabrication and utilization.
Artificial intelligence and digital dentistry:
Artificial intelligence (AI) is transforming digital dentistry in several impactful ways:-
- Diagnostics and Imaging: - AI algorithms can analyse dental images, such as X-rays and CT scans, to detect issues like cavities, bone loss, and tumours with high accuracy. This speeds up diagnosis and improves precision.
- Treatment Planning: - AI can assist in creating customized treatment plans by analysing patient data and predicting outcomes. For example, in orthodontics, AI can help design braces and aligners based on individual patient needs.
- Predictive Analytics :- AI can analyse large datasets to predict potential future issues, such as the likelihood of tooth decay or gum disease, allowing for early intervention and personalized prevention strategies.
- Virtual Simulations: - AI-powered software enables virtual simulations of dental procedures, allowing both patients and practitioners to visualize outcomes before actual treatment begins.
- Robotic Assistance: - In some cases, AI-driven robots are used in procedures for greater precision, such as in implant placement or complex surgeries.
- Patient Management: AI can streamline administrative tasks, manage patient records, and enhance communication between patients and dental practices.
AI in Diagnosis:
A) Enhanced Image Analysis:-
AI algorithms analyse dental images (like X-rays, CT scans, and intraoral scans) to detect abnormalities such as cavities, bone loss, and tumours.
These algorithms can often identify issues that might be missed by the human eye, increasing diagnostic accuracy.
b)Automated Detection :- AI tools can automatically identify and classify dental conditions, such as caries or periodontal disease, by comparing patient images with a vast database of previously diagnosed cases.
c) Risk Assessment: - AI systems can evaluate a patient's overall oral health and predict future issues based on historical data, lifestyle factors, and genetic information, allowing for early intervention.
AI in Treatment:-
A) Planning personalized Plans:-
AI can analyse a patient’s data to create personalized treatment plans. For instance, in orthodontics, AI helps design custom braces or aligners by assessing the patient’s dental structure and predicting how teeth will move over time.
B) Predictive Modelling: - AI algorithms can simulate various treatment scenarios and predict outcomes. This helps in selecting the most effective treatment plan by evaluating potential success rates and adjusting plans based on predicted results.
c) Efficiency and Precision:-
AI aids in precise planning for complex procedures such as implants and surgeries by integrating data from various sources to ensure accurate placement and alignment.
d) Treatment Simulation: - AI-powered software allows for virtual simulations of treatments, enabling both practitioners and patients to visualize and understand the potential results before actual procedures are performed.
Diagnostic Tools:-
A) Digital Radiography:-
Digital X-rays offer faster imaging, reduced radiation exposure, and enhanced image quality compared to traditional film X-rays. They allow for immediate analysis and easy sharing.
b) Intraoral Cameras:-
These small cameras capture detailed images of the inside of the mouth, helping to diagnose issues like cavities, cracks, and plaque build-up. The images can be displayed in real-time, aiding in patient education and treatment planning.
c) Cone Beam Computed Tomography (CBCT):-
CBCT provides 3D imaging of the dental structures, including teeth, bones, and soft tissues, offering a comprehensive view for accurate diagnosis and treatment planning, especially in complex cases like implants.
d) Optical Scanners:-
Digital impressions using optical scanners capture detailed 3D images of the teeth and oral cavity, improving accuracy and comfort compared to traditional melds. Treatment Planning
e) Tools CAD/CAM Systems:-
Computer-Aided Design and Computer-Aided Manufacturing (CAD/CAM) systems are used to design and fabricate dental restorations such as crowns, bridges, and veneers.
F) Simulation Software:-
This software allows for the virtual modelling of various treatment scenarios, helping practitioners and patients visualize potential outcomes before proceeding with actual treatment.
g) 3D Printing:-
Used for creating precise dental models, surgical guides, and even custom prosthetics, 3D printing allows for rapid production and customization, enhancing both treatment efficiency and patient comfort.
H) Digital Workflow Integration:-
Integrated software systems streamline the entire workflow, from initial diagnosis through to treatment and follow-up, facilitating better coordination and data management within the practice.
I) Other Notable Technologies: - This technology enables remote consultations and follow-ups through video conferencing and digital communication, expanding access to dental care and allowing for more flexible patient management.
j) Artificial Intelligence: - AI enhances diagnostic accuracy, aids in treatment planning, and improves practice efficiency by analysing large datasets and offering predictive insights.
AI and digital dentistry have significantly impacted patient care and outcomes in several ways:-
1. Improved Diagnostic Accuracy early Detection:-
AI algorithms can analyse images and data with high precision, leading to earlier detection of dental issues such as cavities, periodontal disease, and oral cancers. Early diagnosis often results in more effective treatment and better outcomes. Reduced Human Error: AI reduces the likelihood of missed diagnoses and increases the consistency and reliability of diagnostic results.
2. Enhanced Treatment Planning personalized Care:-
AI helps create highly individualized treatment plans by analysing comprehensive patient data, including imaging, genetic information, and medical history. This personalization improves the effectiveness of treatments. Predictive Outcomes: AI models can simulate various treatment scenarios and predict outcomes, allowing for more informed decision-making and better alignment of treatments with patient needs.
3. Increased Efficiency and Precision faster Processes:-
Digital tools like CAD/CAM and 3D printing streamline the creation of dental restorations and prosthetics, reducing the time needed for procedures and minimizing patient waiting times.
Accurate Procedures: Technologies such as digital impressions and robotic assistance in surgeries enhance the precision of treatments, leading to better-fitting restorations and reduced procedural errors.
4. Enhanced Patient Experience comfort and Convenience:-
Digital impressions and virtual consultations reduce the discomfort and time associated with traditional methods. -Patients benefit from a more comfortable and efficient care experience. Better Communication: AI-driven simulations and visualizations help patients understand their conditions and treatment options more clearly, leading to more informed consent and satisfaction.
5) Proactive and Preventive Care predictive Analytics:-
AI can analyse patterns and predict potential dental issues before they become severe, enabling proactive preventive care and reducing the need for more extensive treatments later. Tailored Prevention: Digital tools can help in creating personalized prevention plans based on a patient’s specific risks and conditions.
6. Streamlined Practice Management efficient Workflow:-
Integration of digital tools and AI into practice management systems enhances operational efficiency, allowing for better scheduling, record-keeping, and patient management. Data-Driven Insights: AI provides valuable insights from patient data, helping practices to improve their services and patient care strategies.
Transition from the Concept to Clinical Application:-
Transitioning from a concept to clinical application in healthcare or biomedical research involves several stages, each requiring careful planning, testing, and regulatory approval.
1. Conceptualization and Research
2. Ethical and Regulatory Considerations:
3 .Impact
Transition Research into Practice:--Translating research into practice involves several key steps to ensure that evidence-based findings are effectively applied in real-world settings.
-Here is an overview of the main steps:-
1. Identify the Evidence
2. Assess the Context and Need
3. Adapt the Research for Implementation
4. Develop an Implementation Strategy
5. Engage and Train Stakeholders
6. Pilot the Intervention
7. Evaluate and Measure Outcomes
1) Steps involved in translating research into practice:-
Translating research into practice, often referred to as knowledge translation or implementation science, involves several key steps. Here is an overview of the process:-
1. Identify Relevant Research Findings
2. Engage Stakeholders
3. Develop Implementation Strategies
2) Role of clinical trial and evidence based dentistry
Clinical trials and evidence-based dentistry (EBD) are fundamental components of modern dental practice, aimed at improving patient outcomes through scientific research and data-driven decision-making.
Role of Clinical Trials in Dentistry:-
1. Preclinical Research
2. Phase I Trials
3. Phase II Trials
4. Phase III Trials
5. Phase IV Trials
6. Challenges and Strategies for successful implementation.
Strategy implementation can be a complex process that involves translating strategic plans into actions and achieving desired outcomes. However, several challenges can arise during the implementation phase. Here are some common challenges:
1) Resistance to Change:-
Employees or stakeholders may resist the strategic changes due to fear, uncertainty, or a preference for the status quo.
2) Lack of Clear Communication:-
If the strategic objectives, goals, and action plans are not effectively communicated throughout the organization, employees may misunderstand or misinterpret them.
3) Resource Constraints:-
Insufficient resources, such as budgetary constraints, limited staff, or inadequate technology, can impede successful strategy implementation.
4) Lack of Accountability: - Without clear roles, responsibilities, and accountability mechanisms, it can be challenging to ensure that individuals and teams take ownership of their assigned tasks and deliver results.
The 6 key strategy implementation steps:-
1. Define your goals.
2. Conduct proper research.
3. Map out any risks.
4. Schedule all milestones.
5. Assign tasks.
6. Allocate helpful resources.
Future prospects and conclusion:-
Future prospects and provide a conclusion, it's important to first understand the context—whether it's about a career, industry, technology, or something else. Here’s a general guide for crafting these sections
Future prospects:-
1) Analysis of Trends
2) Opportunities for Growth
3) Challenges Ahead
4) Long-Term Sustainability
1) Summary of key finding and advancement:-
Key Findings:-
- Core Insights: - Summarize the most important discoveries or conclusions from your research or analysis.
- Data and Evidence: - Highlight any supporting data or evidence that strengthens these findings.
- Relevance to the Field:- Explain how these findings affect the broader context, whether it's a specific industry, scientific field, or social issue
- Advancements:-
- Technological Breakthroughs: - Outline any major innovations or technological progress.
- Process Improvements: - Mention any advancements in processes or practices that have improved efficiency, accuracy, or outcomes.
- New Applications: - Describe how these advancements are being applied in practical ways.
2) Potential Future Breakthroughs in oral Health Therapies
Oral health is rapidly evolving due to advances in science and technology. Here are some key areas where we might see major breakthroughs shortly:
1) Regenerative Dentistry
2)3D Printing and Personalized Dentistry
3) Nanotechnology in Oral Care
4) CRISPR and Gene Editing
5) Advanced Diagnostic Tools
6) Preventative and Probiotic Treatments
The future of oral health therapies is incredibly promising, with innovations ranging from regenerative dentistry and gene editing to advanced materials and personalized care.
3) Conducting Remark and Implications for Clinical Practice:
The evolving landscape of oral health therapies presents a future where treatments could be more preventive, personalized, and less invasive. Breakthroughs in regenerative dentistry, nanotechnology, CRISPR gene editing, and advanced diagnostics signal a shift from traditional repair-based models to more proactive and biologically integrative approaches. As we move toward biomimetic materials, 3D printing, and oral microbiome management, dentistry could witness a reduction in the prevalence of oral diseases, a longer lifespan for dental restorations, and the development of therapies that promote natural regeneration rather than replacement
Implications for Clinical Practice:
1) Shift toward Preventive Care
2) Personalized Treatment Plans
3) Integration of Regenerative
Conclusion:
Emerging therapies in oral health offer transformative potential to revolutionize the prevention, treatment, and management of a wide range of oral diseases. With innovations in biotechnology, regenerative medicine, and biomaterials, these therapies not only enhance the effectiveness of traditional treatments but also introduce novel, minimally invasive alternatives. Stem cell therapies, gene editing, antimicrobial agents, and advanced restorative materials are among the most promising developments, providing new avenues for addressing issues such as tooth decay, gum disease, and tissue regeneration. As ongoing research leads to improved understanding and implementation of these technologies, it is expected that they will increasingly become integral components of oral healthcare, improving patient outcomes, enhancing quality of life, and offering more sustainable solutions. The continued integration of these emerging therapies into clinical practice will likely define the future of oral health, making it more personalized, efficient, and accessible.
ACKNOWLEDGMENT
We are thankful to Arihant College of Pharmacy, Ahilyanagar. For providing us with the platform and infrastructure for preparing this article also thanks to our Principal Dr. Yogesh Bafana sir, and Assistant professor Ms. Sneha Kanase Mam & Mr. Swapnil Kale Sir for their support and expert opinion during the writing process.
REFERENCE
- Beall CJ, Mokrzan EM, Griffen AL, Leys EJ. Cultivation of Peptidiphaga gingivicola from subgingival plaque: the first representative of a novel genus of Actinomycetaceae. Molecular Oral Microbiology. 2018a; 33(1):105–10. [PMC free article] [PubMed]
- Bedpan-Russo A, Leme-Kraus AA, Vidal CMP, Teixeira EC. An overview of dental adhesive systems and the dynamic tooth-adhesive interface. Dental Clinics of North America. 2017; 61(4):713–31. [PubMed]
- Belli R, Wendler M, de Ligny D et al. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dental Materials. 2017; 33(1):84–98. [PubMed]
- Bendsoe M, Sigmund O. Topology Optimization: Theory, Methods and Applications. 2nd ed. New York: Springer-Verlag; 2004.
- Berdasco M, Esteller M. Clinical epigenetics: seizing opportunities for translation. Nature Reviews Genetics. 2019;20(2):109–27. [PubMed]
- Berdy B, Spoering AL, Ling LL, Epstein SS. In situ cultivation of previously uncultivable microorganisms using the ichip. Nature Protocols. 2017;12(10):2232–42.
- Centers for Disease Control and Prevention, Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to2011-2016, 2019, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Atlanta, GA. https://www.cdc.gov/oralhealth/publications/OHSR-2019-index.html (Accessed 21 June 2023).
- D Selvaraj, S Curtan, T Copeland, et al. Caries disparities among Medicaid-enrolled young children from pediatric primary care settings J Public Health Dent, 81 (2) (2021), pp. 131-142, 10.1111/jphd.12423
- 3)NZ. Bashir Trends in the prevalence of dental caries in the US pediatric population 2011–2020 J Clin Pediatr Dent, 46 (5) (2022), pp. 51-57, 10.22514/jocpd.2022.007
- E. Bouchery Utilization of dental services among Medicaid-enrolled children Medicare Medicaid Res Rev, 3 (3) (2013), pp. E1-E16, 10.5600/mmrr.003.03.b04
- R. J. Lamont, Z. R. Fitzsimonds, H. Wang and S. Gao, J. Periodontol., 2022, 89, 154–165
- I. Mäkinen, V. Y. Pappalardo, M. J. Buijs, B. W. Brandt, A. A. Mäkitie, J. H. Meurman and E. Zaura, Microbiome, 2023, 11, 171
- G. D. Sepich-Poore, L. Zitvogel, R. Straussman, J. Hasty, J. A. Wargo and R. Knight, Science, 2021, 371, eabc4552
- G. El Tekle and W. S. Garrett, Nat. Rev. Cancer, 2023, 23, 600–618
- N. Mohamed, J. Litlekalsoy, I. A. Ahmed, E. M. H. Martinsen, J. Furriol, R. Javier-Lopez, M. Elsheikh, N. M. Gaafar, L. Morgado, S. Mundra, A. C. Johannessen, T. A. H. Osman, E. S. Nginamau, A. Suleiman and D. E. Costea, Front. Cell. Infect. Microbiol., 2021, 11 Search
- Y. Zong, Y. Zhou, B. Liao, M. Liao, Y. Shi, Y. Wei, Y. Huang, X. Zhou, L. Cheng and B. Ren, Front. Cell. Infect. Microbiol., 2021, 11 Search
- B. A. Helmink, M. A. W. Khan, A. Hermann, V. Gopalakrishnan and J. A. Wargo, Nat. Med., 2019, 25, 377–388
- W. Song, A. C. Anselmo and L. Huang, Nat. Nanotechnol., 2019, 14, 1093–1103
- J. Sun, F. Chen and G. Wu, ISME J., 2023, 17, 1535–1551
- E. Elinav, R. Nowarski, C. A. Thaiss, B. Hu, C. Jin and R. A. Flavell, Nat. Rev. Cancer, 2013, 13, 759–771
- J. Hou, M. Karin and B. Sun, Nat. Rev. Clin. Oncol., 2021, 18, 261–279
- S. Mignani, J. Rodrigues, H. Tomas, M. Zablocka, X. Shi, A.-M. Caminade and J.-P. Majoral, Chem. Soc. Rev., 2018, 47, 514–532 RSC.
- T. Li, T. Akinade, J. Zhou, H. Wang, Q. Tong, S. He, E. Rinebold, L. E. Valencia Salazar, D. Bhansali, Y. Zhong, J. Ruan, J. Du, P. Dalerba and K. W. Leong, Adv. Sci., 2022, 9, 2203949
- Sequeira, J. F. Neves, D. Carrero, Q. Peng, N. Palasz, K. Liakath-Ali, G. M. Lord, P. R. Morgan, G. Lombardi and F. M. Watt, Nat. Commun., 2018, 9, 3437
- J. Nam, S. Son, L. J. Ochyl, R. Kuai, A. Schwendeman and J. J. Moon, Nat. Commun., 2018, 9, 1074 CrossRef PubMed.
- P. Zhao, M. Wang, M. Chen, Z. Chen, X. Peng, F. Zhou, J. Song and J. Qu, Biomaterials, 2020, 254, 120142.


 Divya Gore*
Divya Gore*


 10.5281/zenodo.14250419
10.5281/zenodo.14250419